blocked fallopian tube symptoms

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
blocked fallopian tube symptoms

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
At around 10 weeks of pregnancy, many women suddenly notice that their early pregnancy symptoms begin to fade. The morning sickness lessens, the breast tenderness reduces, and the constant fatigue starts to lift. For some, this brings relief — for others, it sparks worry.
If you’ve found yourself thinking, “My 10 weeks pregnancy symptoms gone — is something wrong?”, you’re not alone. At EIRMED, we support thousands of women through fertility and pregnancy journeys. In most cases, this change is a normal and healthy sign of your body adjusting to pregnancy hormones. Let’s explore what this means scientifically and when it’s best to reach out to your healthcare provider.
By week 10, your body and baby are both changing fast. The baby is about the size of a strawberry and developing vital organs, bones, and joints. Internally, your hCG (human chorionic gonadotropin) and progesterone levels — the hormones responsible for many early pregnancy symptoms — start to stabilize.
This hormonal shift is often the main reason why your 10 weeks pregnancy symptoms gone. As your placenta takes over hormone production, your body doesn’t react as strongly to hormonal changes, leading to milder or fewer symptoms.
At EIRMED, we see many women who got pregnant with help from fertility treatments. If that is you, know that your pregnancy might need extra checks. But at 10 weeks, things are often stable. Talk to your doctor about tests like blood screens for issues like Down syndrome. These can also tell the baby’s sex if you want to know.
According to medical experts, yes — it’s completely normal for early pregnancy symptoms to lessen around weeks 9–11.
This phase marks a transition period where your body is adapting beautifully. Nausea, breast soreness, and fatigue may decrease as your hormones level out and your placenta begins supporting your baby’s growth independently.
Many women feel certain signs at this stage. These come from hormones like hCG, which is high now. Here are some usual ones:
Not everyone has all these. Some have strong ones, others mild. If you had them and now notice 10 weeks pregnancy symptoms gone, read on to learn why.
However, a sudden and complete loss of symptoms — especially with bleeding or cramps — should always be discussed with your doctor. While it’s rare, these could signal a complication that requires medical attention.
Understanding why your symptoms change can help ease anxiety. Here are expert-backed explanations for why you may feel better around week 10:
During early pregnancy, high levels of hCG cause symptoms like nausea and vomiting. Around 10 weeks, hCG peaks and then gradually declines, which naturally eases symptoms.
Once the placenta matures, it begins producing hormones needed to sustain pregnancy. This stabilizes your body’s response and lessens discomfort.
Your body adjusts to hormonal and metabolic changes over time. What once felt overwhelming is now manageable as your system adapts.
Balanced nutrition, hydration, and rest can make a major difference. Many women report fewer symptoms after improving their diet or taking prenatal vitamins.
If the loss of symptoms comes with pain, bleeding, or dizziness, it’s important to visit your doctor immediately. They can check your baby’s heartbeat through an ultrasound for reassurance.
Not all changes are bad, but watch for other signs. If symptoms stop fast and you have bleeding, even light spots, tell your doctor right away. Bleeding can be pink, red, or brown. It might come with cramps in your belly or back, like strong period pains. Passing tissue or clots is a big warning.
Other things to note: Severe pain on one side, fever, or bad smell from fluid. These could mean an ectopic pregnancy, where the baby grows outside the uterus. This is rare but needs quick help.
If you had fertility treatments, like IVF, you might worry more. At EIRMED, we know this. We offer products for female fertility, like supplements to boost health. But always check with your doctor. They can do an ultrasound to see the baby’s heart beat. At 10 weeks, it should be strong, like 120 to 160 beats a minute.
Many women share stories online. Some say symptoms went away at 10 weeks, but scans showed all was fine. Others had a loss. The key is to get checked if unsure. Better to be safe.
While it’s normal for pregnancy symptoms to fade, there are certain warning signs that require medical attention. Contact your healthcare provider if you experience:
Vaginal bleeding or spotting
Sharp abdominal or lower back pain
Passing tissue or clots
Dizziness or fainting
Persistent cramping with no other symptoms
At EIRMED, our fertility specialists emphasize that even if everything turns out normal, it’s always better to get checked for peace of mind. Your health and emotional comfort matter.
By 10 weeks, your baby’s development is in full swing. Major organs such as the brain, liver, and kidneys are forming. The arms and legs start moving, though you won’t feel them yet. The baby’s heart is beating strongly — often detectable through an ultrasound.
So, even if your 10 weeks pregnancy symptoms gone, your baby continues to grow and thrive inside you.
Many women describe mixed emotions when early symptoms fade. You might feel relieved to finally eat normally but worried that something might be wrong.
Remember: emotional ups and downs are common during this stage. Hormone shifts can affect mood, but reassurance from your healthcare team and self-care — like gentle exercise, rest, and emotional support — can make a big difference.
If your symptoms fade suddenly, follow these steps before worrying:
Symptom changes are normal. Track how you feel for a few days.
Watch for pain, bleeding, or unusual discharge — these matter more than nausea or fatigue alone.
A quick ultrasound can confirm your baby’s heartbeat and ensure your pregnancy is progressing well.
Continue eating balanced meals, taking prenatal vitamins, and resting adequately.
Most early pregnancy symptoms peak between weeks 6 and 9, then start fading by weeks 10 to 14. Once you reach the second trimester, your energy levels usually rise, and you may start feeling more like yourself again.
This is often called the “golden period” of pregnancy — enjoy it!
Even if your 10 weeks pregnancy symptoms gone, you can promote a healthy pregnancy by:
Eating nutrient-rich meals – Include fresh fruits, vegetables, lean proteins, and whole grains.
Taking prenatal supplements – Especially folic acid, calcium, and iron.
Hydrating well – Drink plenty of water throughout the day.
Staying active – Gentle walks or prenatal yoga can help circulation and stress relief.
Resting adequately – Sleep helps both physical and emotional well-being.
Avoiding harmful substances – Skip alcohol, caffeine, smoking, and any non-approved medications.
These small habits go a long way in ensuring your and your baby’s health.
Fertility experts, including those at EIRMED and leading reproductive centers like CCRM and Illume Fertility, agree that mild changes in pregnancy symptoms are rarely cause for concern. Every pregnancy follows its unique pattern.
Regular prenatal check-ups, early communication with your doctor, and following medical guidance ensure both safety and confidence in your pregnancy journey.
This article aims to support and reassure expecting mothers who notice their 10 weeks pregnancy symptoms gone. It combines expert insights, medical explanations, and emotional care to help you understand what’s normal, what needs attention, and how to stay confident in your pregnancy journey.
Yes, it can be normal. Around 10 weeks of pregnancy, your hormone levels start to balance as your placenta takes over hormone production. This can make symptoms like nausea, fatigue, and breast tenderness fade. However, if symptoms suddenly stop and you feel worried, contact your doctor for a quick check-up.
There are many harmless reasons your symptoms may ease at this stage. Every pregnancy is unique. For most women, it simply means the body is adjusting to new hormone levels. Still, if your symptoms disappear suddenly or you notice spotting, pain, or cramping, it’s best to reach out to your healthcare provider.
Not always. Many people feel “less pregnant” after week 10 because the early hormone surge has passed. But if you have no symptoms and notice unusual changes (such as heavy discharge or bleeding), it’s safer to get medical advice to rule out any concerns.
Morning sickness often fades by week 10–12 for many expectant mothers. It’s usually a positive sign that your body is adapting well. If you’re eating and hydrating normally, and you feel fine otherwise, there’s usually no need to worry.
Yes, symptoms can vary from day to day. Some mornings you may feel great, and others you might feel tired or queasy again. This is completely normal as hormone levels continue to shift during early pregnancy.
You should contact your doctor right away if your pregnancy symptoms disappear suddenly and are followed by:
Vaginal bleeding
Severe abdominal pain or cramping
Dizziness or fainting
These could be signs of complications like a missed miscarriage or hormonal imbalance that needs medical attention.
Not always. Some women lose symptoms naturally, and the pregnancy continues normally. But if symptom loss happens together with spotting, cramps, or a drop in pregnancy test line darkness, consult your doctor immediately for reassurance and a scan.
Absolutely yes! Many women report few or no symptoms by week 10 and go on to have perfectly healthy pregnancies. What matters most is your baby’s growth during check-ups and ultrasound results — not the number of symptoms you feel.
Video Title: 10 Weeks Pregnant What to Expect: Changes for You & Baby
In this video the host covers what happens around the 10-week mark in pregnancy, including how your body is changing, what symptoms you might notice or may be fading, and what’s going on with your baby’s development. It includes sections about how the placenta begins to take more over from early pregnancy hormone surges, which can explain why some symptoms ease. The video also gives tips on what to check with your doctor and how to care for yourself during this transition period.
This content is for educational and informational purposes only. It does not replace professional medical advice, diagnosis, or treatment. Always consult your qualified healthcare provider for any medical questions about your pregnancy.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Help get pregnant over counter pills are a popular choice for many couples looking to boost their fertility in a simple way. When couples are trying to get pregnant, the search for ways to improve success often leads to store shelves full of over-the-counter (OTC) vitamins and supplements. These pills promise to “boost fertility” or “enhance conception.” However, it is essential to look past marketing claims and rely only on what scientific research has proven to be effective and safe.
Scientific evidence divides these supplements into two main categories:
When you’re actively trying to conceive, it’s natural to look for every possible advantage. Many couples wonder about those easily accessible over-the-counter (OTC) pills and supplements that claim to boost fertility. Do they truly work, or are they just hype?
At EIRMED, we believe in providing clear, research-based information. While there are no non-prescription “fertility drugs” designed to replace medical treatments, a specific category of OTC products—dietary supplements—can play a vital, supportive role in optimizing both male and female reproductive health. This guide breaks down what science says about these supplements and how they can be a helpful part of your conception journey.
It is important to understand that over-the-counter supplements are generally nutritional supports, not prescription medications like Clomid or Letrozole, which directly stimulate ovulation or adjust hormones.
However, research shows that deficiencies in certain vitamins and minerals can hinder the quality of eggs and sperm, affect hormonal balance, and disrupt the menstrual cycle.1 Taking the right supplements can correct these deficiencies and provide the essential building blocks for a healthy conception. This is often the first step many fertility specialists recommend.
A woman’s journey to conception requires good egg health, regular ovulation, and a supportive uterine environment.
| Supplement | What it is & How it Helps (Science-Based) |
| Folic Acid (Folate/Vitamin B9) | Crucial for DNA Synthesis. Most famous for preventing neural tube defects in a developing baby, sufficient folate intake before conception is vital for the health and integrity of egg DNA. Health organizations recommend all women of childbearing age supplement with it. |
| Coenzyme Q10 (CoQ10) | Powerful Antioxidant. CoQ10 levels naturally decline with age. This antioxidant is essential for energy production within the egg cell. Studies suggest CoQ10 supplementation may improve egg quality, especially in women with diminished ovarian reserve or those over 35. |
| Myo-Inositol | Supports Ovarian Function. A naturally occurring sugar that is particularly effective for women with Polycystic Ovary Syndrome (PCOS). Research indicates myo-inositol can help improve insulin sensitivity, which often leads to more regular ovulation and better egg quality. |
| Vitamin D | Hormonal Regulation. Low Vitamin D levels are common and have been linked to poorer fertility outcomes. Maintaining sufficient Vitamin D is associated with improved hormone balance and higher pregnancy rates. |
It takes two to tango! Male factor infertility, often related to sperm health (count, motility, and morphology), is a common issue. Antioxidant-rich supplements can protect sperm from cellular damage, known as oxidative stress.2
| Supplement | What it is & How it Helps (Science-Based) |
| Zinc | Sperm Production and Function. Zinc is critical for the structure and function of sperm. Deficiency is associated with low testosterone levels, poor sperm quality, and reduced motility. |
| L-Carnitine and Acetyl L-Carnitine | Sperm Energy and Motility. These amino acids help convert fat into energy and are highly concentrated in healthy sperm. Studies suggest supplementation can improve sperm motility (how they swim) and overall function. |
| Coenzyme Q10 (CoQ10) | Sperm Protection. As an antioxidant, CoQ10 helps protect sperm DNA from oxidative damage, which is key for maintaining high-quality sperm concentration and motility. |
| Selenium & Vitamin E | Antioxidant Team. Selenium is an essential trace element that, when combined with Vitamin E, acts as a powerful antioxidant, protecting the sperm cell membrane and improving sperm motility. |

Certain OTC supplements have shown powerful results, but only in women who have been diagnosed with a specific underlying condition. These are high-dose therapies that should be discussed with a specialist.
CoQ10 is a natural antioxidant that acts as an “energy booster” for cells. It is vital for the mitochondria, the powerhouses inside cells, and is especially important for egg cells, which require a lot of energy for successful fertilization and early development.
Research strongly links CoQ10 supplementation to better outcomes for women over 35 or those with Diminished Ovarian Reserve (DOR)—meaning a low number of remaining eggs.
Studies have shown that CoQ10 pre-treatment, often when combined with fertility treatments like IVF, is significantly correlated with :
The dosages found to be effective in scientific research are high, often around 600 mg daily. This high-dose approach usually needs to be taken for at least 60 days to affect the maturing egg.
Myo-inositol (MI) is often recommended for women diagnosed with Polycystic Ovary Syndrome (PCOS), a common hormonal disorder that leads to irregular or absent ovulation.
MI helps the body become more sensitive to insulin. By improving this insulin response, MI can help to balance hormones, which in turn helps restore regular menstrual cycles and spontaneous ovulation.
For women with PCOS, MI can help regulate the menstrual cycle and may improve the success rate of spontaneous pregnancies. When used during IVF, MI has also been shown to improve the fertilization rate. The recommended dose typically ranges from 2 to 4 grams daily.
Vitamin D is crucial for overall immune and hormonal function. Scientific reviews have associated low levels of Vitamin D (below 30 ng/mL) with an increased risk of infertility.
Supplementation appears to improve the clinical pregnancy rate, but primarily in infertile women who have a confirmed Vitamin D deficiency. For women with PCOS, Vitamin D supplementation has been shown to contribute to higher pregnancy and ovulation rates.
Before focusing on any specialized supplement, every woman trying to conceive should start taking a high-quality prenatal vitamin.3 Prenatals are specifically formulated to provide the basic, necessary levels of nutrients—especially Folic Acid, Iron, and other B vitamins—that support both pre-conception health and early fetal development. It’s an easy, foundational step to ensure your body has what it needs.
While most fertility supplements are safe and beneficial in recommended doses, they are not a substitute for a medical diagnosis.
Always discuss any supplement regimen with your healthcare provider or a fertility specialist to ensure it’s safe and right for your unique situation. Your doctor can also test for nutrient deficiencies to tailor your supplement plan more effectively.
Title: Over-The-Counter Supplements May Improve Fertility
Channel: CBS Boston
Short Description: The video discusses an over-the-counter supplement called Preg Prep, which is marketed to improve the odds of conceiving [00:00]. The supplement has two components: Vita Prep (a multivitamin with B12, D, and folic acid) and Fertile Prep (which supposedly helps sperm reach the egg) [00:14]. An infertility specialist notes that there is no clear scientific evidence that the components work, either alone or in combination, suggesting it may be a waste of money better spent on proven, FDA-approved medications and therapies [00:38]
The information provided by EIRMED on over-the-counter pills and supplements for fertility is for informational and educational purposes only. It is not intended as medical advice, diagnosis, or treatment. Dietary supplements are not regulated by the FDA with the same rigor as pharmaceutical drugs.6 Always consult with a qualified healthcare professional, such as your OB-GYN or a Reproductive Endocrinologist, before starting any new supplement, especially when trying to conceive or if you have any pre-existing medical conditions. EIRMED is not responsible for any adverse effects resulting from the use of products mentioned.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Caffeine is, without doubt, the most widely consumed stimulant worldwide, relied upon by millions of people daily to improve alertness and concentration. When a couple decides to start trying to conceive (TTC), lifestyle and dietary choices immediately come under sharp scrutiny. Among these choices, consumption of caffeine while trying to get pregnant generates significant questions regarding safety and potential effects on reproductive success.
This report serves as an authoritative resource, translating complex scientific findings published in peer-reviewed journals into clear, easy-to-understand guidance. The objective is to move beyond speculation and present only what the available research proves about caffeine’s impact on both male and female fertility and, critically, on the success of an early pregnancy.
One of the most essential aspects of this research involves understanding the critical window of risk. Many individuals assume that strict restrictions on caffeine begin only after a positive pregnancy test has been confirmed. However, scientific evidence clearly demonstrates that the phase leading up to conception and the initial weeks afterward—specifically the time when the embryo is traveling toward the uterus and implanting—are profoundly sensitive. Studies show that caffeine exposure before implantation can severely compromise the outcome. Therefore, lifestyle adjustments must ideally begin the moment a couple starts preparing to conceive, not weeks later after a missed period.
To understand why caffeine is a concern during the pre-conception phase, it is necessary to examine how it behaves biologically and how quantity affects risk.
Caffeine is quickly absorbed into the bloodstream after consumption, reaching peak concentrations relatively rapidly. It is important to remember that individuals process caffeine at different speeds. Variations in caffeine metabolism exist, often influenced by genetics. For some people who are highly sensitive, even doses as low as 100 to 200 mg of caffeine daily may be sufficient to prompt pregnancy complications. This wide variation means that a general safety guideline must be conservative to account for individuals who are particularly susceptible to caffeine’s effects.
The primary biological mechanism that links caffeine consumption to reproductive risk is its role as a vasoconstrictor. Simply put, caffeine causes blood vessels to tighten or narrow. This tightening effect is why caffeine can occasionally help alleviate certain types of headaches, but it has significant implications for reproductive health.
Research, including studies conducted in both pregnant animals and humans, indicates that caffeine increases vascular resistance in the uterus and subsequently reduces the blood flow vital to that area. Reduced uterine blood flow has been suggested to alter the menstrual cycle, potentially shortening the duration of menses. More importantly, reduced blood flow is detrimental to the environment required for a successful pregnancy, as the uterine lining needs rich support, oxygen, and nutrients to successfully prepare for and receive an implanting embryo.
The most consistent finding across reproductive health studies is the Dose-Response Rule: the level of risk is almost always directly related to the amount (dose) of caffeine consumed.6 Low to moderate consumption is generally associated with minimal risk, while high or very high consumption correlates strongly with negative effects, including delayed conception and increased pregnancy loss. This principle forms the foundation of all clinical recommendations, emphasizing that moderation is key.
Research regarding female fertility and caffeine intake primarily focuses on two areas: how long it takes to conceive (Fecundability) and the success rates of fertility treatments.
Some research suggests a link between high caffeine consumption and the time it takes for a woman to become pregnant. For example, a large European study found that women who consumed more than 500 mg of caffeine per day experienced longer times to conception. Conversely, pooled data on moderate consumption (100 mg and 400 mg per day) showed only a relatively small overall effect on reduced Fecundability (the monthly chance of getting pregnant).
It is important to acknowledge that the data on female conception rates are not perfectly consistent. While many studies warn of the risk of high doses, one preconception cohort study found that total caffeine intake among females was not associated with Fecundability, although total male intake was.9 This suggests that the impact of caffeine on a woman’s ability to conceive might be less consistently proven than its impact on the embryo’s ability to survive the first few weeks (i.e., preventing miscarriage). However, given the potential risks later in the process, adopting a conservative limit remains the expert recommendation.
An interesting finding reported in some studies is the potential role of tea consumption. One analysis suggested that higher caffeinated tea intake was associated with a slight reduction in Fecundability among females.9 However, another study found that higher tea consumption was linked to a reduced risk of infertility, where drinking one additional cup of tea per day was associated with a 27% lower risk.6 This mixed finding may be due to the generally lower caffeine concentration in tea compared to coffee, or perhaps the beneficial antioxidant properties found in tea, which could help counteract oxidative stress.
For women undergoing assisted reproductive technology (ART), such as In Vitro Fertilization (IVF) or Intrauterine Insemination (IUI), the evidence regarding caffeine is particularly compelling. Clinical data strongly suggests that women consuming more than 200–300 mg of caffeine per day face nearly twice the risk of not achieving a successful live birth. Conversely, women who maintain a very low intake, specifically less than 100 mg, have a significantly lower risk.
This quantifiable impact on the outcome of expensive and emotionally demanding fertility treatments provides a profound justification for limiting intake. Given the high stakes involved in ART cycles, most fertility clinics routinely advise patients to drastically reduce or eliminate caffeine, as higher intakes, such as more than 400 mg per day, may increase the risk of failure even further.
Reproductive health is a shared responsibility, and the research is increasingly clear that the male partner’s consumption of caffeine while trying to get pregnant plays a significant role in the couple’s success.
High levels of caffeine intake in men are associated with a reduced likelihood of conception. Paternal consumption exceeding 700 mg per day has been linked to a reduced likelihood of conception. Furthermore, studies have shown that total caffeine intake among males at $\geq 300$ mg per day is associated with reduced fecundability (the monthly chance of pregnancy). Based on these findings, specialists recommend that men aim to consume no more than 200 mg of caffeine daily while attempting conception.
High caffeine consumption has been consistently linked to negative impacts on fundamental sperm quality 10:
Perhaps the most worrying finding regarding male consumption is the link between high caffeine intake and increased damage to the sperm’s DNA, known as DNA fragmentation.10 DNA integrity is absolutely essential for the healthy development of the resulting embryo. High levels of DNA fragmentation can lead directly to lower overall fertility rates and, critically, potentially higher miscarriage rates, even if fertilization is achieved.
This biological link underscores that the male partner’s caffeine habits affect not just the chance of getting pregnant, but the chance of sustaining the pregnancy. This confirms that caffeine reduction is truly a couple’s effort, as the quality of the genetic material contributed by the father impacts the viability of the early embryo.
It is worth noting that while some bodies, such as the American Society for Reproductive Medicine (ASRM), have stated that moderate caffeine consumption has no apparent effect on semen parameters in men 7, the detailed mechanistic studies showing increased DNA fragmentation, reduced motility, and reduced count 6 suggest that adopting a conservative limit is the safest, most prudent course of action for sperm health.
The period immediately following fertilization and leading up to implantation is one of the most fragile stages of pregnancy, and research has identified clear biological pathways through which caffeine interferes with these events.
Caffeine’s fundamental role as a vasoconstrictor provides the biological bridge connecting consumption to adverse pregnancy outcomes. Reduced blood flow to the uterus, caused by the tightening of blood vessels 5, means the uterine lining may not be adequately supported. Studies using animal models have demonstrated that caffeine exposure directly impairs the readiness of the uterus to accept the embryo, a condition known as compromised uterine receptivity.
This effect occurs specifically during the pre-implantation stage, making the womb less welcoming before the embryo has had a chance to fully settle.
Beyond affecting the uterine lining, caffeine exposure has been shown to impair the embryo itself. Research indicates that caffeine disrupts the normal movement of the embryo through the fallopian tube (oviductal embryo transport). It also disrupts the subsequent development of the embryo, often resulting in aberrant or failed implantation.
The fact that embryo transport and development are compromised before implantation occurs (which typically happens 6 to 10 days after conception) reinforces the necessity of reducing caffeine intake while actively trying to conceive, long before a woman is aware that she is pregnant.
The most severe documented outcome associated with high caffeine intake is an increased risk of pregnancy loss. High consumption, defined as approximately 3.5 to 7 cups of coffee or generally above 200–300 mg per day, is associated with a substantially higher risk of losing the pregnancy. This link is biologically plausible because of the established disruption to uterine blood flow and embryo development documented in early stages.
While the strength of this link is sometimes debated (for instance, the American College of Obstetrics and Gynecology, ACOG, noted conflicting studies where some found a doubling of risk over 200 mg/day and others found no increase 11), the overall evidence points toward prudence. Because of the established biological mechanisms—impaired implantation and compromised blood flow—public health recommendations strongly advise limiting caffeine intake to low levels during the preconception period and pregnancy.
Based on the scientific evidence detailing risks to sperm quality, conception time, implantation, and early pregnancy survival, a clear consensus emerges regarding maximum daily limits for couples attempting to conceive.
Major reproductive and medical health bodies, including the ASRM and ACOG, generally concur that moderate caffeine consumption poses no apparent adverse effects on fertility or pregnancy outcomes. This moderate consumption is typically defined as 1 to 2 cups of coffee or less than 200 milligrams (mg) of caffeine per day.
For women, this 200 mg limit acts as a crucial safety measure, mitigating the increased risk of miscarriage seen when consumption rises above this threshold.4 For men, specialists strongly recommend consumption remain at or below 200 mg daily to preserve optimal sperm DNA integrity and motility.
Given the potential for severe adverse effects, especially implantation failure and early loss, even at relatively low levels for sensitive individuals 4, experts recommend that couples trying to conceive take the most conservative approach possible to maximize their chances.
The table below synthesizes the established scientific limits into practical risk categories for couples attempting to achieve pregnancy:
Caffeine Intake Levels and Associated Reproductive Risk
| Daily Caffeine Intake (mg) | Equivalent (Approx. Standard Coffee Cups) | Observed Risk Level (TTC Couple) | Key Scientific Findings (Male & Female) |
| Less than 100 mg | 1 standard cup or less | Minimal to Low Risk (Ideal Goal) | No apparent adverse effects on fertility or pregnancy outcomes. Recommended conservative target. |
| 100 mg to 200 mg | 1 to 2 standard cups | Moderate Risk (Acceptable Limit) | General maximum limit for women TTC. Risk of complications may begin for sensitive individuals.4 Recommended maximum for men TTC.6 |
| 200 mg to 300 mg | 2 to 3 standard cups | Increased Concern (Monitor Closely) | Threshold where miscarriage risk begins to rise significantly for women. Reduced male fecundability seen at this level. |
| More than 300 mg | 3+ standard cups | High Risk of Adverse Effects | Associated with substantially higher risk of pregnancy loss and delayed female conception. Linked to poor sperm quality (motility, DNA damage). |
Adopting the 200 mg limit requires couples to understand where caffeine comes from and how to track their total intake accurately.
While most adults may safely consume up to 400 mg of caffeine per day for general health 1, this limit is reduced when attempting to conceive. It is crucial for couples to recognize that caffeine is found in more than just traditional coffee.
A particularly serious concern involves high-concentration caffeine products, such as powdered or liquid caffeine. The U.S. Food and Drug Administration (FDA) warns that these products can deliver toxic and lethal levels of caffeine; for instance, just one teaspoon of powdered caffeine is equivalent to roughly 28 cups of coffee. These products must be strictly avoided by everyone, particularly those attempting pregnancy.
The table below provides a conservative estimate of the caffeine content in common items to help couples manage their daily allowance:
Practical Caffeine Content Guide
| Beverage/Item | Typical Serving Size | Estimated Caffeine Content (mg) | Actionable Advice for TTC Couples |
| Brewed Coffee (Drip) | 8 fl oz (1 cup) | 95–200 mg | Max 1-2 small cups per day; use the higher end for calculation. |
| Espresso Shot | 1 fl oz | 63–75 mg | Lattes/Cappuccinos often contain multiple shots; track total shot count carefully. |
| Decaffeinated Coffee | 8 fl oz (1 cup) | 2–5 mg | Excellent substitution; contains small residual caffeine. |
| Black Tea | 8 fl oz (1 cup) | 25–48 mg | Generally safer; associated with lower infertility risk. |
| Cola Soda | 12 fl oz can | 30–40 mg | Males should limit/avoid; often linked to reduced fertility. |
| Energy Drink | 8 fl oz | 70–160 mg | Should be avoided due to high, variable levels and often harmful additives. |
While total milligram intake is the primary factor, the source of caffeine may also be important, especially for male fertility. Research has highlighted that caffeinated sodas and energy drinks, specifically, are associated with reduced male Fecundability. This finding suggests that the issue may not stem from the caffeine alone, but rather from the high concentration of caffeine combined with other ingredients commonly found in these processed beverages, such as excessive sugar or artificial additives.
Since high caffeine consumption may increase oxidative stress—damage to the body’s cells, including sperm 10—maintaining a balanced diet rich in antioxidants (found in fruits, vegetables, and nuts) is a supportive strategy that can help counteract this stress.
Limiting caffeine is one part of a comprehensive strategy for optimizing reproductive health. Both men and women should be encouraged to maintain a healthy lifestyle, which includes avoiding smoking, limiting alcohol use, ensuring adequate sleep, and avoiding exposure to known reproductive toxins.7 Women should also take a daily folic acid supplement (400 $\mu$g) while trying to conceive. By viewing caffeine restriction as an element within a broader health plan, couples maximize their physical readiness for conception.
The body of scientific research regarding caffeine while trying to get pregnant reveals consistent patterns of risk, particularly when consumption exceeds moderate levels. The evidence is robust enough to establish clear guidelines for maximizing the chances of conception and minimizing the risk of early pregnancy loss.
Dr. Natalie Crawford, an OBGYN and REI specialist, breaks down caffeine’s role in fertility and early pregnancy, including limits to avoid miscarriage risks. Ideal for women planning conception, with tips on monitoring intake for optimal reproductive health.
Video Link: Ep 95 Caffeine & Your Fertility: Does It Really Matter?
Queries (What People Are Asking) |
Core Answers |
| How much caffeine is safe when trying to conceive? | Limit to less than 200 mg per day. (About 1-2 cups of brewed coffee.) |
| Does coffee affect implantation? | Some evidence suggests high intake may interfere with embryo attachment or increase miscarriage risk; 200 mg is the safe cut-off. |
| Do I need to quit coffee entirely while TTC? | No, complete abstinence is not required; moderation (<200 mg) is the key recommendation. |
| Caffeine and miscarriage risk pre-conception | Consumption over 200 mg to 300 mg (especially in the early weeks) is associated with a slightly higher risk. |
| What foods have caffeine I should avoid when TTC? | Energy drinks, large specialty coffees, and sometimes soda/tea are high-risk sources; check labels. |
| Does caffeine affect male fertility? | High intake (often over 300 mg) is sometimes linked to lower sperm quality and motility; men should also moderate. |
| How much caffeine in a Starbucks latte is safe? | It varies greatly; most standard shots are 75 mg; a large brewed coffee can often exceed the 200 mg limit in one cup. |
| Can one cup of coffee a day hurt fertility? | No, one cup of coffee (typically 95 mg to 150 mg) is widely considered safe and does not appear to impact fertility rates.Disclaimer Section |
This article offers general facts for learning and is not medical advice. See a healthcare provider for your own situation on fertility matters. EIRMED does not give diagnoses or treatments. Outcomes differ for each person. We are not responsible for choices made from this info. Always get expert care for health.
This article is for general knowledge only and not medical advice. Always see a healthcare provider for your symptoms or treatments. EIRMED products aid health but do not cure. Results can differ. We use info from public sources, but check with pros for your needs.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Tips for conceiving with one fallopian tube can make a big difference if you are trying to start or grow your family. Many women worry when they learn they have only one working tube, perhaps after surgery or an infection. But the good news is that pregnancy is still possible. Your body is smart—an egg from either ovary can travel to the open tube.
As a fertility expert, I see this often. In this article, we will cover what you need to know, from basic facts to simple steps you can take at home. We will also talk about when to get help from a doctor. At EIRMED, our website helps with products for both male and female fertility, like vitamins that support egg health. Think of this as a friendly chat to guide you. Let’s look at how you can boost your chances.
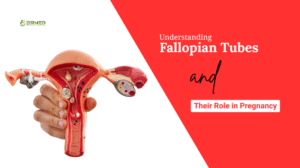
Fallopian tubes are thin paths that connect your ovaries to your uterus. Each month, an ovary releases an egg, and the tube catches it. Sperm swims up to meet the egg there for fertilization. If all goes well, the fertilized egg moves to the uterus to grow into a baby.
Sometimes, one tube gets blocked or removed. This might happen from an ectopic pregnancy, where the baby grows in the tube instead of the uterus. Or it could be from infections like pelvic inflammatory disease, or even surgery for endometriosis. About 1 in 4 women with fertility issues have tube problems, based on what doctors see.
But with one healthy tube, your body can adapt. The open tube can pick up eggs from both sides. Studies show many women get pregnant naturally this way. It might take a bit longer, but it happens. Knowing this can ease your mind as you plan.
The diagnosis of having only one functioning fallopian tube—known medically as Unilateral Tubal Patency (UTP)—can understandably cause concern regarding fertility. However, the foundational scientific evidence offers strong reassurance: having one open tube does not typically halve the chances of conceiving. The reproductive system often demonstrates remarkable adaptability.
For patients who have undergone treatment or surgery related to tubal issues, the outlook remains positive. Research analyzing patient outcomes, even those involving intervention for obstruction, has shown that individuals presenting with unilateral obstruction had a post-intervention conception rate of approximately 41%. This robust statistic highlights that the body can compensate effectively, and the capacity for pregnancy remains high. The critical message supported by clinical data is one of optimism: conception, whether spontaneous or assisted, is highly probable, provided the remaining tube is healthy and ovulation is occurring regularly.
A common belief is that conception can only occur during cycles when the ovary on the same side as the working tube releases the egg. This would mean that roughly every other month is a “wasted” cycle. Scientific investigation into reproductive physiology strongly contradicts this belief.
The pelvis is a fluid-filled cavity, and the released egg (oocyte) is not immediately captured by the nearest tube. Once the egg is released from the ovary, it enters the surrounding pelvic space, allowing the single functional fallopian tube to move and sweep across the pelvic floor to locate and collect the egg, regardless of which ovary produced it. This ability of the egg to be collected by the contralateral (opposite-side) tube is a well-documented phenomenon known as Contralateral Ovum Pick-up, often referred to as the “Wanderer Egg” effect in simpler terms.
Clinical studies have provided precise data on the frequency of this biological compensation. Among women who have had one tube surgically removed (salpingectomy) and successfully conceived naturally, approximately one-third of these pregnancies are the result of the egg being picked up from the ovary opposite to the remaining, functioning tube.2 Specifically, this rate is cited as being around 32% to one-third of reported cases.
This finding is critically important because it confirms that the single working tube is highly efficient. Furthermore, analysis of the natural cycle shows that the cycle length and the hormonal profiles—including levels of Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), and progesterone—are independent of the site of ovulation.3 In simple terms, the body does not favor or select the ovary on the side of the open tube. Ovulation is typically a random event, occurring equally often on the side with the tube and the side without it.
The combination of these two physiological facts maximizes natural conception chances: because ovulation is random and occurs every month, and because the functional tube can successfully collect the egg from the opposite side a high percentage of the time, the individual is fertile during every ovulatory cycle, not just 50% of the time. This inherent biological efficiency provides a strong scientific basis for continued, persistent, and well-timed natural conception efforts before resorting to more complex treatments.

When fertility relies on a single transportation system (the remaining tube), optimizing overall systemic health becomes crucial. Evidence-based lifestyle adjustments do not just improve the quality of eggs and sperm; they also ensure the single fallopian tube functions at its absolute best.
Maintaining a healthy internal environment is fundamental to conception success. Several lifestyle factors are scientifically linked to optimized reproductive function.
Achieving and maintaining a healthy body weight is paramount. Being significantly overweight or underweight can disrupt the delicate hormonal balance necessary for reproduction. Specifically, extreme deviations in weight can prevent the regular release of eggs (a condition called anovulation) and lead to irregular menstrual cycles.
While exercise is beneficial, excessive, hard physical activity, particularly for individuals who are already at a healthy weight, may affect ovulation and can lower levels of the hormone progesterone. Moderation is key to supporting regular ovulatory cycles.
Exposure to certain environmental toxins and lifestyle habits directly compromises fertility:
The importance of eliminating these factors is amplified in the context of unilateral tubal patency. Smoking and poor health cause oxidative stress and inflammation. The success of the single working tube relies on the incredibly delicate, hair-like structures inside it (cilia) that must move the egg and sperm. These delicate mechanisms are highly sensitive to inflammation. Therefore, optimizing systemic health ensures the single remaining tube is operating at its peak mechanical capacity to successfully execute the “Wanderer Egg” pickup.
A correct balance of proteins, carbohydrates, and lipids in the daily diet provides essential benefits for optimal female reproductive health.5 Nutritional science emphasizes the importance of specific micronutrients:
While stress itself is not considered a primary cause of infertility, it can negatively impact overall health.4 Managing stress through techniques like meditation, deep breathing, or yoga supports the body’s optimal function during the conception effort. Furthermore, constantly working the night shift might disrupt hormone levels and raise the risk of lowered fertility. If night work is necessary, ensuring sufficient sleep when not working is recommended.
For individuals relying on one working tube, precision in timing sexual intercourse is necessary to ensure sperm are present when the egg is released.
A crucial tool for timing is the at-home urine Ovulation Predictor Kit (OPK). This kit detects the surge, or sudden release, of Luteinizing Hormone (LH) in the urine. The LH surge is the signal that causes the ovary to release the egg.6 By tracking this surge, individuals can pinpoint their fertile window, which typically includes the two to three days leading up to, and the day of, ovulation.
For those engaging in low-tech treatments such as Intrauterine Insemination (IUI) (discussed in Part III), timing is even more strictly monitored using transvaginal ultrasound. This imaging technique allows doctors to view the ovaries and measure the growth of developing eggs (follicles).6 In clinical settings, medication such as a human chorionic gonadotropin (HCG) injection may be administered to trigger ovulation at the exact moment required for IUI.

For many individuals with unilateral tubal patency who have not conceived naturally after a period of trying, the next step involves low-tech fertility treatments that combine oral medications with timed placement of sperm (IUI).
Simple oral medications, such as Clomiphene Citrate (Clomid) or Letrozole, are commonly used to induce Controlled Ovarian Stimulation (COH). The goal of COH is to encourage the ovaries to release more than one egg in a single cycle. By increasing the number of eggs available, the statistical chance of at least one egg traveling successfully and being collected by the single functioning tube is enhanced.
Clomiphene Citrate is very successful at its primary task: approximately 80% of women who take Clomid successfully ovulate.7 However, the overall success in achieving pregnancy is lower, at around 40%.7 This difference demonstrates that while medication successfully generates the egg, the ability of the fallopian tube to transport the egg and sperm and support early conception remains the limiting factor.
The effectiveness of COH combined with IUI declines significantly with age. In cycles involving IUI for unexplained infertility (a situation often compared to unilateral patency with a healthy tube), the pregnancy rate per cycle showed a clear decrease: it was 11.5% for women aged 35–37, dropping to 7.3% for women aged 38–40, and further declining to 4.3% for women aged 41–42.7 These rates show that while these treatments are viable, the window of maximum effectiveness closes quickly with advancing age.
IUI is a procedure where, after ovarian stimulation, a specially prepared, highly concentrated sample of motile sperm is placed directly into the uterus using a thin catheter.8 The sperm still must swim from the uterus into the functional fallopian tube to meet the egg.
The key scientific finding for patients with unilateral tubal patency is that the success of IUI is highly dependent on where the blockage occurred in the non-functional tube. This distinction—whether the blockage is proximal or distal—is determined by a diagnostic test, typically Hysterosalpingography (HSG).
A proximal blockage is located close to the point where the fallopian tube enters the uterine wall.
Prognosis: Patients with a proximal block have a generally positive prognosis for IUI combined with COH. Multiple studies, including meta-analyses, show that infertile patients diagnosed with a proximal unilateral tubal blockage (UTB) can expect cumulative pregnancy rates (CPRs), or overall success, after COH-IUI that are statistically similar to those of control groups (patients who have bilateral tubal patency but unexplained infertility).9 Clinical evidence shows similar pregnancy rates per cycle and similar cumulative pregnancy rates when compared to controls.10 This suggests that if one tube is blocked proximally, the remaining open tube is likely healthy and fully capable of facilitating pregnancy.
A distal blockage is located at the end of the tube, near the ovary. This often indicates a more serious underlying issue, such as hydrosalpinx, where the tube becomes blocked and filled with fluid.
Prognosis: Patients with distal unilateral tubal blockage have a significantly poorer prognosis for IUI. Clinical data reveals substantially lower success rates compared to women with unexplained infertility.11 For example, studies tracking three cycles of IUI showed CPRs of only 11.7% for patients with distal blockage, compared to 44.7% for controls.11 Patients with distal blockage had significantly lower cumulative pregnancy rates than controls.10
The stark difference in success rates reveals the pathology behind the tubal damage. A proximal blockage often represents a less serious mechanical issue, such as a spasm during the HSG test or a minor physical obstruction that does not affect the health of the remaining tube or the uterine environment.
In contrast, distal blockage is associated with widespread damage to the tube itself, often caused by past infections. If the blocked tube is distally damaged and contains inflammatory fluid (hydrosalpinx), that fluid can sometimes leak back into the uterus. This toxic, inflammatory fluid is known to inhibit embryo implantation or harm sperm, making the uterine environment hostile to conception, even if the other tube is technically open and functional.
Therefore, the scientific proof dictates that if distal blockage is confirmed, repeating IUI cycles is medically inefficient and financially wasteful. For these patients, In Vitro Fertilization (IVF) should be considered as the more appropriate approach to bypass the damaged structure entirely.
The following table summarizes the critical findings regarding IUI success based on the location of the tubal issue, offering a clear guide for strategic decision-making.
IUI Success Rates Based on Location of Tubal Issue
| Location of Tubal Issue | Likely Condition of the Remaining Tube | Expected IUI Success (3 Cycles) | Key Scientific Finding |
| Proximal Blockage (Blockage near the uterus) | Remaining tube is likely healthy and clear. | Good chance; similar success rates to women with unexplained infertility. | Cumulative Pregnancy Rates (CPRs) are statistically similar to controls.9 |
| Distal Blockage (Blockage near the ovary) | Often indicates damage (like hydrosalpinx) or severe inflammation. | Significantly lower chance of success. | CPRs are notably reduced (44.7% vs 11.7% for distal); IVF is often recommended.10 |
For patients with unilateral tubal patency, successful treatment requires a strategy that includes clear stopping points for low-tech methods and a predetermined transition to high-tech methods.
Intrauterine Insemination (IUI) is usually the first line of clinical treatment due to its lower cost and invasiveness compared to IVF. However, studies show diminishing returns over time.
Clinical consensus, supported by financial analysis, suggests that after three unsuccessful cycles of IUI, the probability of any subsequent cycle working drops significantly.12 This finding establishes the “three cycle rule” as a standard clinical guideline for determining when to shift treatment protocols.
On a per-cycle basis, IUI is significantly more affordable than IVF.12 However, focusing only on the per-cycle cost can be misleading. The more relevant metric is the cost per live birth.
If a patient falls into a category with an extremely poor prognosis for IUI (such as those with distal tubal blockage), the odds of birth are close to zero.12 In such cases, repeating IUI cycles becomes an “incredibly poor option,” resulting in wasted financial resources and, critically, wasted time. Once a patient passes the three-cycle limit without success, IVF often becomes the more affordable and efficient option on a per-birth basis because the probability of success per IVF cycle is vastly higher than for a subsequent IUI cycle.
In Vitro Fertilization (IVF) completely bypasses the need for the fallopian tube. The process involves retrieving the eggs from the ovaries, fertilizing them with sperm in a laboratory, and then transferring the resulting embryo directly into the uterus. This direct placement eliminates the mechanical requirement for the fallopian tube to function, thereby maximizing the chances of conception when tubal function is compromised.
Based on the evidence, IVF is the superior or immediate choice in specific clinical scenarios:
A historical factor leading to the loss of one fallopian tube is often a previous ectopic pregnancy (a pregnancy implanted outside the uterus). Although ectopic pregnancy generally affects only about 1 in 100 pregnancies, individuals who have experienced one are understandably sensitive to the risk of recurrence.
The risk of a recurrent ectopic pregnancy is a crucial consideration, especially if the previous surgical management involved a partial removal of the tube. Recurrence is rare, but it can occur in the remaining, distal portion of the ipsilateral (same-side) fallopian tube following a proximal salpingectomy (partial removal).
For patient safety, medical and surgical experts recommend performing a total salpingectomy (complete removal of the damaged tube) whenever an ectopic pregnancy is managed surgically, or if IVF is chosen and the remaining tube shows damage.13 A thorough review of past surgical records is necessary to confirm whether the original surgery was a partial or total removal, as this significantly impacts future risk assessment.
It is important to note that if a severe distal blockage (hydrosalpinx) is identified in the remaining tube, even if the plan is to pursue IVF, removal or surgical clipping of that tube may be recommended by the specialist. This is not because the tube is needed for IVF (it is not), but because the toxic fluid contained within the damaged tube can leak into the uterus, compromising the optimal environment required for an IVF-created embryo to implant successfully. Maximizing the chances of implantation is necessary to justify the time and financial investment of IVF.
The most effective strategy for conceiving with unilateral tubal patency is one that is guided by diagnostic imaging (HSG) results, monitors age, and establishes clear transition points between treatment types. The strategy must leverage the body’s natural compensatory ability while quickly shifting to high-tech solutions when mechanical or pathological barriers are present.
The final summary roadmap integrates all major scientific findings regarding blockage location, IUI limits, and the transition to IVF, ensuring an efficient and evidence-based pathway to conception.
Evidence-Based Treatment Roadmap for One Fallopian Tube
| Clinical Scenario | Initial Recommended Approach | Scientific Rationale (Why it works) | When to Shift Treatment (Next Step) |
| Natural Conception Attempt (Unilateral Patency Confirmed) | Focus on Lifestyle Optimization and Timed Intercourse. | High chance of “Wanderer Egg” pick-up (approx. 32%).2 Overall conception rate is favorable.1 | After 6-12 months of timed attempts, or earlier if age requires faster intervention. |
| Confirmed Proximal Blockage (Near the Uterus) | Controlled Ovarian Stimulation (COH) + IUI. | Success rates (CPRs) are similar to standard unexplained infertility cases.9 This is the most cost-effective first step.12 | After 3 unsuccessful cycles of IUI, transition to IVF.12 |
| Confirmed Distal Blockage (Near the Ovary, e.g., Hydrosalpinx) | Proceed directly to IVF. | IUI success rates are severely impaired (e.g., only 11.7% CPR) due to probable structural damage and potential toxicity.10 | IVF is the primary recommendation. Consider tubal removal/clipping before IVF to ensure successful embryo implantation. |
| Advanced Age (e.g., over 38) | Proceed directly to IVF, or limit IUI to 1-2 cycles. | Need for the highest possible success rate per cycle to conserve critical time and egg quality due to rapidly diminishing odds after age 38.7 | IVF is the primary recommendation to maximize efficiency. |
Conceiving with only one fallopian tube is a very realistic goal, supported by robust clinical data. The human reproductive system demonstrates a powerful compensatory mechanism, allowing the single working tube to successfully collect eggs released by the opposite ovary in approximately one-third of cases. Therefore, the first step should always involve maximizing natural potential through precise timing and optimal lifestyle health, particularly focusing on maintaining a healthy weight and eliminating toxins like tobacco.
When medical intervention is necessary, the decision between Intrauterine Insemination (IUI) and In Vitro Fertilization (IVF) is dictated almost entirely by the anatomical findings. Patients with proximal tubal blockages can expect good success with IUI protocols, comparable to couples facing unexplained infertility. However, the presence of a distal blockage significantly lowers the probability of IUI success, making immediate transition to IVF the scientifically recommended and financially pragmatic choice.
By using this evidence-based roadmap, individuals with unilateral tubal patency can pursue conception with a clear, strategic, and optimized plan tailored specifically to their physiological circumstances.
Video Link: HOW TO GET PREGNANT WITH ONE TUBE? Causes, Treatment of blocked tube & possibility of conception
This 15-minute video by a doctor discusses causes of blocked fallopian tubes, effective treatments, and practical tips for conceiving with one tube, including natural methods and fertility options. It’s clear and supportive, ideal for women navigating this challenge—aligning with EIRMED’s focus on products like ovulation kits and supplements to boost your chances.
Yes, pregnancy is absolutely possible with one fallopian tube, as long as you have at least one healthy ovary, regular menstrual cycles (indicating ovulation), and no other fertility issues. Studies show up to 85% of women with one healthy tube can conceive naturally within a year if under 35. The remaining tube can even “pick up” eggs from the opposite ovary due to the body’s natural adaptability. If you’ve had an ectopic pregnancy or surgery, monitor for scarring. Real users on Reddit report successful pregnancies within 3-6 months post-tube removal, often by tracking ovulation.
Your chances are good—around 66% within one year for healthy women, rising to 85% over two years, compared to 85% in the first year with two tubes. Factors like age (higher success under 35), overall health, and the reason for tube loss (e.g., ectopic vs. infection) play a role. If the remaining tube is blocked or scarred, it may drop to 15-20% per cycle. Tips include maintaining a healthy weight and avoiding smoking to optimize odds. Many Reddit users conceive from the “tubeless” side, showing the body’s compensation.
Tracking ovulation is a top tip for conceiving with one fallopian tube, as it ensures timing intercourse during your fertile window (days 10-17 of a 28-day cycle). Use ovulation predictor kits (OPKs), basal body temperature (BBT) charting, or apps like Flo. Cervical mucus changes (clear and stretchy) also signal peak fertility. Since you ovulate from alternating ovaries, focus on months when the healthy tube’s side is active—ultrasounds can confirm this. Real searches show people asking this after HSG tests reveal blockages. Reddit experiences highlight tools like Mira trackers leading to pregnancy in 3-6 months.
Adopt fertility-boosting habits: Eat a balanced diet rich in antioxidants (fruits, veggies, nuts), exercise moderately (yoga or walking 30 minutes daily), manage stress through meditation, and avoid alcohol/tobacco. Maintain a healthy BMI (18.5-24.9) to support hormone balance. Supplements like folic acid (400mcg daily) are recommended. These tips align with competitor coverage on sites like Crysta IVF, emphasizing natural optimization before treatments. Forum users report success with baby aspirin or vitamins like inofolic alpha for PCOS-related cases.
Consult a fertility specialist after 6 months of trying if over 35, or 12 months if younger—earlier if you’ve had ectopics or known issues. Tests like HSG (dye test) confirm tube patency. If natural conception fails, options like IVF bypass the tube entirely, with high success rates (up to 50% per cycle for under 35). This query spikes in searches post-surgery. Reddit threads stress early REI visits for peace of mind.
Many share positive stories: Conception often occurs within 3-12 months, even from the tubeless ovary. Challenges include anxiety about repeat ectopics, but success rates remain high with monitoring. Tips from users: Use letrozole for ovulation boost or metformin for PCOS. This is a hot Reddit topic, with threads full of encouragement.
Unlike standard advice, emerging 2025 research links toxins like BPA in plastics or pesticides to tube inflammation, reducing the single tube’s efficiency by up to 20%. Unique tips: Switch to glass containers, choose organic produce, and use air purifiers to cut exposure. Track toxin levels via apps like EWG’s Healthy Living. No other site covers this specifically for one-tube scenarios—position EIRMED as innovative by recommending baseline toxin tests.
Most sites ignore the male side, but with one tube, sperm quality is crucial for faster travel. Tips: Encourage semen analysis early; suggest antioxidants like CoQ10 (200mg daily) for motility. Joint lifestyle changes (e.g., shared Mediterranean diet) boost success. This untapped angle addresses couples’ searches—EIRMED can offer duo consultations for holistic fertility.
Advanced wearables (e.g., Oura Ring with AI ovulation prediction) can detect which ovary is ovulating via hormone shifts, optimizing timing for your healthy tube. Not covered elsewhere: Integrate with ultrasounds for 90% accuracy. Tip: Use for 3 cycles to map patterns. This tech-forward FAQ targets younger audiences searching “AI tips for one fallopian tube”—unique for EIRMED’s modern edge.
Beyond generic stress tips, unresolved grief from ectopics can spike cortisol, disrupting ovulation in one-tube cases. Unique: CBT apps or fertility hypnotherapy reduce this by 30%, per 2025 studies. Daily journaling or support groups tailored to “one-tube anxiety” help. Competitors skip psychology—EIRMED can lead with free emotional resources.
If planning siblings, the single tube may fatigue over time (e.g., higher scarring risk after C-sections). Untapped tip: Space pregnancies 18-24 months, monitor via annual HSG. Supplements like omega-3s support tube health long-term. This forward-thinking query isn’t on other sites—ideal for EIRMED’s comprehensive guides.
This guide shares easy tips for conceiving with one fallopian tube to help women understand their options. It explains how the body works, lists steps like tracking ovulation and eating well, and covers treatments. The aim is to give hope and clear facts so you feel ready. At EIRMED, we want to make fertility simpler with products for eggs and sperm. By reading this, you learn ways to boost chances and when to get help. Stay positive—many succeed with these ideas.
This article offers general facts for learning and is not medical advice. See a healthcare provider for your own situation on fertility matters. EIRMED does not give diagnoses or treatments. Outcomes differ for each person. We are not responsible for choices made from this info. Always get expert care for health.
Thank you for taking time to read these tips for conceiving with one fallopian tube. We hope this information brings you closer to your dream of a family. At EIRMED, we are committed to supporting your fertility needs with quality products. You are strong for seeking knowledge—keep going with hope. Best wishes on your path.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Keys to a successful IUI start with knowing what to do before, during, and after the process. If you are thinking about intrauterine insemination, or IUI, as a way to build your family, you are not alone. Many people turn to this treatment when natural conception is hard. IUI places sperm right into the uterus to help fertilization happen. It is less complex than some other options and can work well for couples dealing with mild fertility issues.
In this guide, we will look at the main factors that can help your IUI go well. We will talk about how to prepare your body, what happens on the day, and tips to care for yourself afterward. As an expert in fertility for both men and women, I want to share this in a simple way, like we are talking over tea. At EIRMED, our site offers products to support your needs, such as supplements for better egg or sperm health.
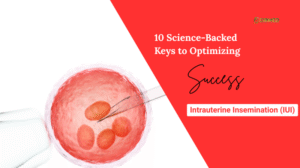
Intrauterine Insemination (IUI) is a popular way to boost the chance of pregnancy. It’s a gentler and often more affordable step before considering complex treatments like In Vitro Fertilization (IVF). In simple terms, IUI involves a doctor placing a concentrated sample of high-quality sperm directly into the patient’s womb (uterus) right around the time the egg is released (ovulation). This procedure helps the sperm skip past the cervix, which is usually a barrier, drastically shortening the distance they need to swim to reach the egg.
Success in IUI isn’t a matter of luck. It depends on carefully planning and perfecting specific factors—including biology, medicine, and procedure steps—that have been proven to work through worldwide clinical studies. By focusing only on the variables with strong scientific proof, patients and their doctors can achieve the best possible results. This report outlines ten research-backed keys that are essential for maximizing the chance of a successful pregnancy with IUI.
The first crucial step in making IUI work is checking the female partner’s overall fertility health. These starting biological factors tell doctors how well a patient will react to the treatment and lay the groundwork for the whole cycle.
The total number of eggs a patient has remaining, known as the ovarian reserve, is a very strong sign of how successful fertility treatment will be. Doctors use two main measurements to find this out: Anti-Müllerian Hormone (AMH) and Antral Follicle Count (AFC).
The AMH test is a quick blood test that gives the most dependable estimate of how many eggs a patient still has. Studies show a clear connection: when AMH levels are high, the chances of IUI success are also higher. One important study found that the chance of clinical pregnancy was twice as high (20.0%) when the patient’s AMH level was greater than 2.1 ng/mL, compared to cycles where the level was lower (10.0%). This simply means that women with a good supply of eggs have a much better likelihood of getting pregnant with IUI.
The Antral Follicle Count (AFC) is used alongside AMH. This count is done using an ultrasound to check how many small, resting egg sacs (follicles) are in the ovaries at the start of the menstrual cycle. A higher AFC means there are more potential eggs that can be encouraged to grow during the stimulation phase. Research confirms that patients who achieve a clinical pregnancy tend to have a noticeably higher mean AFC (about 4.0) compared to those who don’t (about 3.2), with the best starting point often being 3.5.
Checking AMH and AFC before treatment is an essential strategic move. If a patient’s AMH is very low (far below 2.1 ng/mL), it suggests a risk of a Poor Ovarian Response (POR). In these cases, even using strong medications (Key 4) often leads to limited success (sometimes as low as 9.2% in certain treatment groups). For patients with very low egg reserves, IUI might be a waste of valuable time, and they should immediately think about moving to IVF. These markers are not just tests; they are vital tools for creating a personalized treatment plan.
A patient’s age is widely known as the most important biological factor affecting IUI results. This is because the quality and quantity of eggs naturally drop over time, making it much harder to achieve a successful pregnancy as a patient gets older.
The data clearly shows that IUI success rates continuously decrease with age. For women under 35 years old, the IUI success rate per cycle is at its highest, around 13%. This rate dips to 10% for women aged 35 to 37 years. The drop becomes steeper after age 38, with success rates falling to 9%, and decreasing further to between 3% and 9% for patients over 40 years.
This age-related decline dictates the entire treatment strategy. Since time is limited, especially for women aged 38 and above, treatment must be very efficient. For example, spending four to six cycles on a treatment that only offers a 3% to 9% chance per cycle is statistically inefficient compared to quickly switching to a treatment with a higher success rate, like IVF. The goal is to choose the most effective treatment plan as quickly as possible to counter the natural decline in egg quality.
For a fertilized egg to turn into a baby, the lining of the uterus, called the endometrium, must be perfectly ready to accept and support it. The thickness of this lining (EST) is a crucial physical measurement for success in any assisted reproductive procedure, including IUI. If the endometrium is too thin, it may not have the necessary blood flow and support for the egg to implant successfully.
Research has set clear limits for the uterine lining. Studies show an absolute failure zone: no pregnancies occurred when the peak EST was measured at less than 5.1 mm or greater than 15 mm. This means that if the lining falls outside this critical range, the chance of success is zero, no matter how good the sperm or egg are.
For the best outcomes, most doctors aim for an EST that is in the “sweet spot.” A lining of 7 mm to 12 mm is generally linked to higher pregnancy and implantation rates, with 8 mm often seen as the minimum thickness required to move forward with the procedure.
Monitoring the endometrial thickness is therefore a required check before the IUI is performed. Since success is impossible outside the critical thresholds, checking the lining is mandatory. If the lining is poor (e.g., less than 7 mm), the cycle should be stopped or changed, as a perfect insemination performed into an unsuitable environment will always fail.
The next keys focus on getting the medical treatments and steps exactly right during the IUI cycle itself.
A key part of IUI success, especially for unexplained infertility, is controlled ovarian stimulation (COS). This uses medication to encourage the growth of several healthy eggs in one cycle. The drug protocol chosen directly affects the number and quality of the eggs produced.
Scientific evidence strongly supports using protocols that aggressively promote follicle growth. Overall studies have shown that using Gonadotropins alone resulted in higher pregnancy rates (33.33%) compared to regimens combining clomiPHENE Citrate (CC) with Gonadotropins (18.36%). This indicates that a stronger medication strategy generally leads to a better chance of clinical pregnancy.2
The best results are seen when aggressive stimulation matches the patient’s capacity. For women who already showed a high ovarian reserve (AMH greater than 2.1 ng/mL, as seen in Key 1), using a comprehensive stimulation protocol—which includes Clomiphene, human gonadotropins, and an hCG trigger (ChmghCG)—resulted in the highest success rate of 32.1%.
This high success rate proves that using strong drugs works best when the patient’s underlying biology is strong. If a patient’s egg capacity is low (low AMH), using aggressive drugs may not help much, which supports the idea of either using a simpler, cheaper stimulation or moving directly to IVF. For a patient with strong markers, using the optimal, aggressive protocol is the best way to leverage her natural potential.
Once the ovaries have been properly stimulated (Key 4) and the eggs are the right size, the exact timing of the next two steps—the ovulation trigger shot and the sperm injection—is absolutely vital. The egg is only able to be fertilized for a very small window after it is released.
The process begins with an injection of human chorionic gonadotropin (hCG), often called the trigger shot, which causes the final maturation and release of the egg. The IUI procedure must then be strictly scheduled to happen about 36 hours after the hCG trigger shot.9 This timing is essential to ensure that the concentrated sperm sample is already waiting in the fallopian tube precisely when the egg is released, maximizing the chances of fertilization.
Because the window of opportunity is so narrow, the procedure’s timing is non-negotiable. Research suggests that any delay or mistake in scheduling the IUI relative to the hCG injection can significantly lower the success rate. Even with the best eggs and sperm, incorrect timing guarantees failure, which is why sticking to the 36-hour rule is one of the most critical, yet completely controllable, factors for IUI success.
IUI is mainly designed to help sperm reach the egg. Therefore, the quality of the sperm sample and the technical skill used in the procedure are extremely important.
The quality of the prepared sperm sample, measured by the number of actively swimming sperm, is the biggest male predictor of IUI success. This is known as the Total Motile Sperm Count (TMSC), which is the number of active, moving sperm measured after the sample has been washed and concentrated, right before the insemination.
While a few pregnancies have been reported with very low counts, the evidence shows that success rates improve dramatically once the TMSC hits a certain level. Pregnancy rates are significantly better when the post-wash TMSC is at least 5 million. This 5 million mark acts as a crucial minimum for being a good candidate for IUI.
For patients aiming for the highest possible success rate, current research suggests that the chance of pregnancy is best when the TMSC is 9 million or higher. On the flip side, success rates drop sharply when the count is very low; the monthly success rate falls to just 5.3% when the TMSC is below 1 million.
The TMSC is the ultimate check for male fertility issues. If the post-wash count consistently falls below 5 million, IUI is statistically not worth the effort. For couples dealing with severe male infertility, personalized advice should strongly recommend moving to more advanced techniques like IVF with Intracytoplasmic Sperm Injection (ICSI), where the need for high motility is bypassed.
The actual process of injecting the prepared sperm into the uterus demands technical precision to maximize the chance of success.
The main goal of the procedure is to smoothly and completely deposit the concentrated sperm into the uterine cavity, avoiding any damage or the possibility of the sperm flowing back out. Studies have looked into whether the type of catheter used—such as a soft-tip versus a hard-tip—affects the results, but large trials found no significant difference in pregnancy or live birth rates between the two types.
This finding suggests that the specific tool used is less important than the skill and technique of the doctor performing the IUI. The most important technical factor is ensuring the sperm delivery is gentle and accurate. A rough procedure could cause the uterus to contract, which might push the sperm out or prevent its journey toward the fallopian tube. Additionally, standard care often includes resting quietly (lying down) for about 20 minutes after the procedure and receiving luteal support (progesterone) to help keep the uterine environment favorable.
IUI success is closely linked to the patient’s general health and any existing medical conditions. Lifestyle choices can directly affect how well medication works, while specific diagnoses can make the procedure useless.
Lifestyle factors, which are completely controlled by the patient, play a significant role in how effectively the body responds to treatment drugs and prepares the uterus.
Smoking: The scientific evidence against smoking during fertility treatment is very strong. Studies show that patients who smoke need a significantly higher dose of gonadotropin drugs to achieve the same level of ovarian stimulation compared to non-smokers. This increases both the cost and the burden of the treatment. Furthermore, smoking is known to harm the implantation environment by causing a thinner endometrium (EST). A thin lining directly goes against the need for optimal EST (Key 3). By quitting smoking, a patient improves her body’s drug response (Key 4) and enhances the quality of the implantation site (Key 3). Quitting smoking is one of the most effective ways a patient can reduce costs and boost success.
Alcohol: While research found no major link between moderate caffeine intake and fertility success, the findings on alcohol consumption are clearer. A high level of weekly alcohol consumption by women (specifically, greater than 84 grams per week, which is about six standard drinks) is negatively linked to the chance of pregnancy in assisted reproductive technologies. Similarly, high weekly consumption in men (over 84 grams per week) is associated with a decreased live birth rate.
BMI Context: It is important to note that a review of multiple studies on female Body Mass Index (BMI) found that having a high BMI did not statistically change IUI treatment outcomes (clinical pregnancy or live birth rates). Nevertheless, advice on weight loss is often still given to women with a high BMI to lower general pregnancy risks.
IUI is an excellent treatment for specific problems, most often unexplained infertility (the diagnosis in 50.1% of successful cycles studied) and cases where there are issues with sperm delivery. However, IUI is medically ineffective in cases involving severe physical problems within the female reproductive system.
IUI relies on the fundamental step of sperm naturally meeting the egg in the fallopian tube for fertilization. Therefore, the procedure is severely limited, or completely unsuitable, for patients who have:
For patients diagnosed with conditions known to damage fertility (e.g., tubal disease, diminished ovarian reserve), evaluation and treatment should start right away. Continuing IUI when a structural issue exists—like a severely blocked fallopian tube—is scientifically pointless because the sperm cannot reach the egg. This key emphasizes that the initial diagnosis must be a critical checklist item to confirm IUI is the right choice before starting any cycle.
A defining characteristic of a successful fertility journey is knowing when a treatment strategy has reached its peak and confidently moving on to a more effective option. This choice must be based on age and cumulative results, not just emotion.
Fertility specialists generally agree that patients should attempt between 3 and 6 unsuccessful IUI cycles before seriously thinking about moving on to IVF . For women under 35 with no major issues, three to four cycles offer a total success rate of up to 20% to 30% . However, research clearly shows that after four unsuccessful attempts, the chance of success drops significantly .
The cycle limit must be adjusted according to age (Key 2):
| Maternal Age Group | Recommended Limit of Unsuccessful Cycles | Why the Limit is Set (Strategic Rationale) |
| Under 35 years | 3 to 4 cycles | Total success is decent; there is less urgency to rush. |
| 35 to 37 years | 2 to 3 cycles | Age-related decline begins; efficiency must be prioritized. |
| 38 years and older | 1 to 2 cycles, or skip IUI entirely | Rapid drop in egg quality; low success chance per cycle (3-9%). |
The reason for setting this limit is the principle of diminishing returns. Continuing past the recommended limit wastes precious time, particularly for older patients. Since IVF offers a much higher chance of success per cycle, moving to it is not giving up, but rather a logical, evidence-based step toward the ultimate goal of achieving a live birth. Moving to IVF is also strongly recommended sooner if a patient has limited egg reserve (Key 1) or if multiple high-quality IUI attempts (Keys 4, 5, 6) have failed.

The road to a successful IUI cycle is built not just on hope, but on strict adherence to clinical evidence and scientific thresholds. By making the most of biological capacity, ensuring procedural accuracy, and following strict diagnostic rules, couples can significantly increase their chances of success.
The tables below summarize the critical, research-backed numerical targets that define an optimized IUI cycle.
| Marker (Simple Term) | Clinical Measurement | Optimal Target for Best Success | Critical Threshold (High Risk/Failure) |
| Egg Reserve (AMH) | Anti-Müllerian Hormone (ng/mL) | Greater than 2.1 ng/mL | Below 2.1 ng/mL |
| Follicle Potential (AFC) | Antral Follicle Count | Greater than 3.5 | N/A |
| Uterine Lining (EST) | Endometrial Thickness (mm) | 7 mm to 12 mm | Below 5.1 mm or above 15 mm |
| Post-Wash TMSC Range (Millions) | Expected Outcome | Clinical Recommendation |
| Less than 1 million | Very low monthly chance (around 5.3%) | Usually advised to move to IVF/ICSI |
| 5 million or higher | Good candidate profile for IUI (> |
Standard recommendation |
| 9 million or higher | Optimized chance for IUI pregnancy | Best predictive range |
In summary, a successful IUI cycle needs perfect coordination: the patient must have enough eggs (Key 1), be in the appropriate age range (Key 2), have a healthy uterine lining (Key 3), use the strongest possible stimulation protocol (Key 4), perform the insemination at exactly the right time (Key 5), use a strong sperm sample (Key 6), ensure gentle technique (Key 7), follow positive lifestyle habits (Key 8), be an appropriate candidate free of severe structural defects (Key 9), and have the strategic wisdom to switch to IVF when necessary (Key 10). Following these science-backed steps provides the best possible foundation for success.
As a fertility expert at EIRMED, I often recommend trusted videos from board-certified doctors to help couples understand IUI better. These align with what top fertility sites like CCRM and Illume Fertility cover—focusing on preparation, timing, and tips for higher success rates. Here’s a standout one:
Video Link: Maximize Your Chances for Getting Pregnant with Intrauterine Insemination – Dr. Lora Shahine
Sumary of Video: In this 10-minute video, reproductive endocrinologist Dr. Lora Shahine shares practical steps to boost IUI success, including who it’s best for, how the procedure works, and key factors like ovulation timing and lifestyle tweaks. It’s straightforward and hopeful, perfect for couples starting their journey—much like the expert advice we provide at EIRMED for male and female fertility support.
Age is the single most important factor determining IUI success, as egg quality and quantity naturally decrease over time.
Generally, success rates are highest for younger patients and drop significantly as a woman ages:
This continuous decline is why doctors often recommend moving to more advanced treatment (IVF) much sooner for patients over 38.
Doctors measure the quality of the sperm sample after it has been washed and prepared, using a number called the Total Motile Sperm Count (TMSC)—the total number of actively swimming sperm.
While some rare pregnancies occur even with very low counts, research shows that success rates are significantly better when the TMSC is at least 5 million. If the TMSC is 5 million or higher, the pregnancy rate is typically 8.2% or more per cycle.
For the best possible chance of success with IUI, the optimal TMSC is 9 million or higher. If the TMSC drops below 1 million, the monthly chance of success falls sharply to only 5.3%, suggesting that IVF/ICSI may be a more efficient option.
The Anti-Müllerian Hormone (AMH) blood test is the best way to estimate your remaining egg supply (ovarian reserve).
Research has identified a crucial cut-off point of 2.1 ng/mL. Having an AMH level greater than 2.1 ng/mL is associated with a much higher probability of success. Specifically, cycles where the patient’s AMH was above this number had a pregnancy rate of 20.0%, which is double the rate (10.0%) seen in cycles where the AMH level was below 2.1 ng/mL.
For patients with an AMH level above 2.1 ng/mL, using a strong stimulation protocol (like Gonadotropins) can further boost the success rate to 32.1%.
Yes, most fertility experts recommend setting a limit because the chance of success drops significantly after a certain number of attempts.
The limit is strongly dependent on the patient’s age:
| Maternal Age Group | Recommended Limit of Unsuccessful Cycles | Rationale |
| Under 35 years | 3 to 4 cycles | These cycles offer a decent total success rate (up to 20–30%).
|
| 35 to 37 years | 2 to 3 cycles | Moving to IVF sooner is recommended due to the age-related decline in egg quality.
|
| 38 years and older | 1 to 2 cycles, or skip IUI | It is often recommended to move quickly to IVF due to the rapid decline in egg quality and very low success rates (3-9%).
|
If you have completed the recommended number of cycles for your age without success, transitioning to IVF is seen as the next logical and more efficient step.
The uterine lining, or endometrium (EST), must be ready to receive the fertilized egg.
Yes, absolutely. Lifestyle choices you can control play a major role in success:
Quitting smoking and limiting alcohol intake are proven ways to improve your body’s response to medication and prepare the uterus for pregnancy.
IUI is most helpful for couples with unexplained infertility or issues with sperm delivery. However, IUI is ineffective when there are severe structural problems that prevent the sperm and egg from meeting.
IUI has the lowest success rates and is often not recommended if you have:
For patients with these conditions, doctors generally advise moving directly to IVF, as IUI is scientifically unlikely to succeed
This article aims to share simple, helpful facts on keys to a successful IUI. It helps people understand the process, prepare their bodies, and care for themselves after. By covering health checks, lifestyle tips, and emotional support, it meets what users search for. The goal is to make fertility journeys easier and more hopeful. At EIRMED, we want you to feel informed and ready to buy products that fit your needs, like supplements for better results. Stay positive—many find success with these steps.
This content is for general information only and not medical advice. Always talk to a doctor for personal guidance on fertility treatments. EIRMED does not diagnose or treat conditions. Results vary by person. We are not liable for any actions based on this article. Seek professional help for your health needs.
Thank you for reading this guide on keys to a successful IUI. We hope it gives you hope and clear steps for your fertility path. At EIRMED, we are here to support you with quality products. Remember, every journey is unique, and you are taking brave steps. Wishing you all the best.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Abortion pill changed mind refers to a situation where a person takes the first medication for abortion but then decides to continue the pregnancy. The abortion pill, also known as medication abortion, involves two drugs: mifepristone and misoprostol. Mifepristone blocks progesterone, a hormone needed for pregnancy. If only the first pill is taken, there may be options to consider, but action must be quick. This article explains the process, evidence on potential reversal, risks, and next steps based on scientific sources. Data from groups like the American College of Obstetricians and Gynecologists (ACOG) show that claims about reversal lack strong proof. At EIRMED, a site focused on fertility, resources are available for those who choose to proceed with pregnancy. 🔗
Medication abortion uses drugs to end a pregnancy. It is approved for use up to 10 weeks from the last menstrual period in many places. The first drug, mifepristone, stops the pregnancy by blocking progesterone. This causes the uterine lining to break down.
The second drug, misoprostol, is taken 24 to 48 hours later. It causes contractions to expel the pregnancy tissue. The process can involve bleeding and cramps, similar to a miscarriage. Follow-up care checks if it is complete.
This method is done at home or in a clinic. Side effects may include nausea, diarrhea, or chills. It has a success rate of about 95 to 98 percent when both drugs are used as directed. 🔗
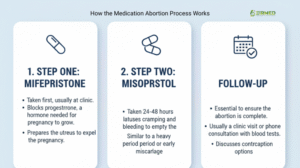
The process begins with a medical check. An ultrasound confirms the pregnancy stage and rules out issues like ectopic pregnancy. Mifepristone is taken orally, often at a clinic.
Misoprostol follows, usually at home. Bleeding starts within hours and can last up to two weeks. A doctor visit or test confirms completion. If not complete, more medication or a procedure may be needed.
Without the second drug, the pregnancy may continue in some cases, but risks exist.
People may change their decision after taking the first pill due to various factors. These can include new information, support from others, or personal reflection. Studies indicate that regret after abortion is uncommon, but feelings can shift.
It is important to assess emotions and seek medical input promptly.
After mifepristone, some may experience light bleeding or no symptoms. If misoprostol is not taken, the pregnancy might persist. Heavy bleeding or severe cramps signal the need for immediate care.
Monitoring symptoms helps determine next actions.
If abortion pill changed mind occurs after mifepristone but before misoprostol, contact a healthcare provider immediately. Provide details on timing and dosage. An ultrasound can assess the pregnancy status. 🔗
Acting within 72 hours is critical, as effects may progress.
Claims of reversing medication abortion involve giving progesterone after mifepristone. Some reports suggest success rates of 64 to 68 percent in case series. However, major medical organizations state there is no reliable evidence it works. 🔗 🔗
A randomized trial was halted due to safety concerns, including hemorrhage, and could not confirm efficacy. ACOG describes it as unproven and not recommended. 🔗
Proponents suggest progesterone counters mifepristone by supporting the uterine lining. It may be given as injections or pills for several weeks.
Evidence comes from observational studies without control groups, which limits conclusions.
Attempts may lead to incomplete abortion, infection, or birth defects if unsuccessful. In one study, participants experienced severe bleeding requiring emergency care. Progesterone side effects include fatigue and mood changes. 🔗
Medical groups advise against it due to insufficient data. 🔗
If choosing to continue, start prenatal care. This includes ultrasounds, blood tests, and vitamins like folic acid. Monitor for complications from the medication.
Adoption services are available if parenting is not preferred. Resources provide counseling on choices.
At EIRMED, fertility products such as supplements are offered for those supporting pregnancy health.
Decision changes can cause stress. Counseling services offer neutral support. Hotlines provide confidential talks.
Mental health care is part of overall well-being during this time.
Schedule exams to check viability. Tests measure hormones like hCG. Watch for signs of infection, such as fever or heavy bleeding.
Emergency care is needed for severe symptoms.
An abortion, whether medical (using medication) or surgical, ends a pregnancy. After the procedure, the body begins to return to its normal reproductive cycle. Ovulation — the release of an egg from the ovary — can resume relatively quickly once hormone levels start to stabilize.
Medical research indicates that ovulation can occur as soon as 2 to 3 weeks after an abortion. In some cases, it may even happen within 8–14 days, depending on the individual’s hormonal response. This means that fertility can return before the next menstrual period, making pregnancy possible quite soon afterward.
Key points:
Most women ovulate around 2–4 weeks post-abortion.
Menstrual bleeding after an abortion is not a reliable sign of fertility status.
Since sperm can survive in the reproductive tract for up to five days, unprotected sex shortly after an abortion can lead to conception.
A woman’s first period typically occurs 4 to 8 weeks after the procedure. This can vary based on factors like:
Type of abortion (medical vs. surgical)
Gestational age at the time of abortion
Hormonal fluctuations
General health and body weight
It’s important to note that bleeding immediately after an abortion is not a menstrual period — it’s the body’s way of expelling tissue and healing the uterus.
Because fertility can return quickly, healthcare providers often discuss contraceptive options right after an abortion. Common choices include:
Hormonal methods: birth control pills, patches, injections, or implants
Barrier methods: condoms, diaphragms
Long-acting reversible contraception (LARC): IUDs or implants (which can sometimes be inserted immediately after a surgical abortion)
If a person wishes to avoid pregnancy, using contraception from the first act of intercourse after the abortion is recommended.
For those who wish to become pregnant again, most medical professionals recommend waiting until:
After at least one normal menstrual cycle, to allow the uterine lining to recover fully.
The person feels physically and emotionally ready.
This isn’t a strict biological requirement — pregnancy is possible earlier — but it’s a practical guideline for monitoring future cycles and ensuring overall health.
Abortion is a medical event that can affect both the body and mind. Physically, most people recover within a few days to weeks. Emotionally, recovery varies widely. Managing stress, seeking support, and consulting healthcare providers about family planning can aid in overall wellbeing and future reproductive health.
Early case reports claimed success, but critiques note flaws like no comparisons. A 2019 trial stopped early over safety, finding no clear benefit.
Ongoing research is needed for better data.
Medication abortion generally does not affect long-term fertility. Most people can conceive later without issues. If concerns arise, fertility evaluations are available.
Healthy habits support reproductive health.
Title: Changed your mind after taking the abortion pill?
Understanding the Abortion Pill
How Abortion Pill Reversal (APR) Works
Safety and Efficacy of APR
If You Want to Reverse the Pill
A: There are three possible outcomes if you only take the first pill (mifepristone) and do not take the second pill (misoprostol):
A: If the pregnancy continues after you take only the first pill, studies show it is unlikely that the mifepristone will cause birth defects or harm the baby later on.
A: It depends. The cost of this treatment (which involves taking extra progesterone) changes based on the type of medication you need and what your insurance plan covers.
A: Pregnancy symptoms do not go away instantly, but they fade quickly.
A: You can ovulate and get pregnant as soon as two weeks after an abortion, but a home pregnancy test may not be accurate for a few weeks.
A: It is completely normal to feel a lot of different emotions at the same time. The most common feelings are:
This guide explains abortion pill changed mind with facts on the process, reversal evidence, and steps to take. It covers risks, options, and health checks from scientific sources. The goal is to inform without bias, helping readers understand choices. At EIRMED, fertility products are available if needed. Always consult doctors for accurate advice based on evidence.
This content is for educational purposes only and not medical advice. Consult a qualified healthcare provider for personal guidance. EIRMED products support fertility but do not guarantee outcomes. Information is based on public sources; individual results vary. Decisions should be made with professional input.
Thank you for reading this information on abortion pill changed mind. The aim is to provide factual details to aid understanding. At EIRMED, resources are available for fertility concerns. Seek professional guidance for your situation.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Intrauterine Insemination (IUI) is a common, non-surgical fertility treatment that places washed and concentrated sperm directly into a woman’s uterus around the time of ovulation. While the procedure itself is quick, the subsequent period, often called the “two-week wait,” is crucial for successful implantation.
To optimize your chances of a successful pregnancy and maintain both your physical and mental well-being during this time, it is important to understand what activities, substances, and habits should be avoided. This article provides essential information on things to steer clear of after your IUI procedure.
IUI is a fertility help where washed sperm goes right into your uterus. This makes it easier for sperm to meet the egg. Doctors do it around the time you ovulate, when an egg comes out. It is less hard than IVF and costs less too.
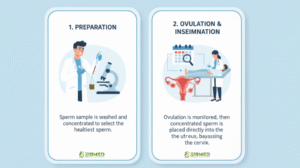
The steps start with meds to help eggs grow, then a shot to release the egg. On the day, it takes just minutes. After, you rest a bit and go home. Many couples try it for issues like low sperm count or unexplained no baby.
At EIRMED, we know IUI can bring hope. Our products for female fertility, like vitamins, can add support.
Certain physical activities can create unnecessary stress on your body or raise your internal temperature (hyperthermia), which may not be ideal during the sensitive implantation window.
| Category | Actions to AVOID | Rationale |
| High-Impact Exercise | High-intensity interval training (HIIT), long-distance running, intense cycling/spin classes, or sports with high risk of abdominal trauma. | Reduces unnecessary jarring, bouncing, or physical stress on the pelvis. |
| Heat Exposure | Hot tubs, saunas, steam rooms, or prolonged exposure to very hot baths. | Excessive heat can raise your core body temperature, which may interfere with early stages of pregnancy/implantation. |
| Heavy Lifting | Lifting extremely heavy weights or objects that cause you to strain. | Minimizes pressure and strain on the abdomen and pelvis following the procedure. |
| Pelvic Activity | Sexual activity that causes pain or intense cramping (follow clinic-specific instructions for intercourse). | Reduces the risk of uterine contractions and discomfort immediately following the IUI. |
Introducing harmful chemicals or substances into your body during the two-week wait can potentially impact implantation or fetal development.
While it is impossible to eliminate all stress, managing your emotional state during the waiting period is vital for your overall well-being. Focus on self-care and distraction.
| Stressor | Habit to BREAK | Positive Action to Take |
| Symptom Hunting | Obsessively analyzing every cramp, twinge, or change as a sign of pregnancy. | Engage in gentle distraction (reading, light hobbies, nature walks). Symptoms of early pregnancy often mimic PMS. |
| Early Testing | Taking an at-home pregnancy test before the date specified by your clinic. | Stick to the scheduled test date. Early testing risks a false negative or a false positive (if you used an hCG trigger shot), leading to unnecessary emotional stress. |
| Excessive Worry | Constant anxiety or “what-if” thinking about the IUI outcome. | Prioritize rest and stress-reducing activities like meditation, deep breathing, or spending time with a supportive partner. |
Intrauterine Insemination (IUI), often called artificial insemination, is one of the most common and lowest-cost ways to treat infertility. If you are starting your fertility journey in Texas, understanding the cost of IUI is key to planning your family.

The price of a single IUI cycle in Texas can vary greatly, generally ranging from $800 to $4,000+ per cycle, not including medication. This wide price range depends on several factors, including the clinic you choose and the type of treatment plan your doctor recommends.
When a fertility clinic quotes a price for IUI, they often give a “base price.” However, a full treatment cycle involves many necessary steps, each with its own cost. The actual total cost of IUI comes from adding up these individual parts.
Here is a simple look at the major cost parts for one IUI cycle in Texas:
This is the price for the main event: preparing the sperm and performing the insemination.
| Service Component | Estimated Cost Range (Per Cycle) | Details |
| IUI Procedure (Insemination) | $300 – $1,000 | The fee for the doctor or nurse to insert the washed sperm into the uterus. |
| Sperm Washing/Prep | $300 – $800 | The lab fee to separate the healthy, moving sperm from the semen fluid for use in the procedure. |
| Total Base Cost | $600 – $1,800 | This is the minimum cost for the procedure and lab work alone. |
To time the IUI perfectly and ensure safety, your doctor must monitor your cycle with blood tests and ultrasounds. These fees often add up quickly.
| Service Component | Estimated Cost Range (Per Cycle) | Details |
| Cycle Monitoring (Ultrasounds & Bloodwork) | $500 – $2,000 | Includes multiple visits to track egg growth and hormone levels. This ensures the IUI is timed correctly around ovulation. |
| Initial Consultation & Testing | $200 – $3,500 | Before your first IUI, you will need tests like a Semen Analysis, hormone checks (AMH), and often an HSG (tubal check). |
| Total Monitoring Cost | Highly Variable | This cost depends heavily on the number of appointments needed and your initial testing. |
The type of medication you take to stimulate your ovaries makes the biggest difference in the final price of the cycle.
| Medication Type | Estimated Cost Range (Per Cycle) | Use Case |
| Oral Drugs (Clomid, Letrozole) | $30 – $200 | Used for mild stimulation; the most common and least expensive option. |
| Trigger Shot (hCG) | $100 – $300 | An injection given to trigger the final release of the egg(s) at a precise time. |
| Injectable Drugs (Gonadotropins/FSH) | $1,500 – $3,500+ | Used for stronger ovarian stimulation; this dramatically increases the cycle cost due to the high price of the medicine. |
Takeaway: For a fully monitored IUI cycle using oral medications and a trigger shot, the “all-in” out-of-pocket cost usually falls in the range of $2,000 to $4,000 in Texas.
The cost of IUI is not fixed. Several factors can either lower the price or cause unexpected costs.
Understanding your health insurance coverage is essential, as this can dramatically reduce your out-of-pocket cost.
While IUI costs are significant, they are much lower than In Vitro Fertilization (IVF). This is why many doctors suggest IUI as a starting point.
| Treatment Type | Average Cost Per Cycle (Texas, Self-Pay) | Complexity |
| IUI Cycle (Monitored & Medicated) | $2,000 – $4,000 | Simple, in-office procedure. |
| IVF Cycle (Full) | $13,000 – $20,000+ | Complex procedure involving egg retrieval and lab fertilization. |
The question of can you have intercourse after IUI is common, and the answer, supported by medical research, is generally yes. Many fertility specialists not only permit but actively encourage timed intercourse following an Intrauterine Insemination (IUI) procedure.

This practice is considered safe and, in certain patient groups, may offer a simple way to slightly improve success rates.
While the IUI procedure places washed sperm directly into the uterus, having intercourse at the right time may provide a physiological “boost” to the conception process.
The timing is what matters most. Experts recommend aligning intercourse with the peak fertility window, which is controlled by the “trigger shot” (hCG injection) used to time ovulation.
| Timing of Intercourse | Scientific/Expert Recommendation | Rationale |
| Night of the hCG Trigger Shot | Encouraged | The trigger shot causes ovulation about 36 hours later. Having sex ensures fresh, natural sperm are in the reproductive tract before the egg is released, covering the full fertile window. |
| Immediately After IUI Procedure | Wait 12–24 Hours | This precaution allows the cervix to close completely and reduces any minor discomfort or slight risk of introducing infection right after the catheter procedure. |
| Day After IUI Procedure | Often Recommended | This timing uses the “natural boost” of uterine contractions and seminal fluid exposure during the period when the egg is most likely to be present (ovulated after the IUI). |
While intercourse is generally safe after IUI, your fertility doctor may advise you to abstain temporarily in the following medical scenarios to prevent complications:
In summary, the medical consensus supports that you can have intercourse after IUI, particularly within 24–48 hours of the procedure, as it is a safe practice that may offer modest benefits, especially in cases with sub-optimal sperm quality.
The video features Dr. Kurt Peterson, a reproductive endocrinologist, who provides a comprehensive guide to the Intrauterine Insemination (IUI) process. The goal of IUI is to place optimized sperm near the time of ovulation to increase pregnancy chances.
Title: IUI Explained | What is the IUI process step by step?
This guide helps you learn things to avoid after IUI to raise your pregnancy chances. It explains why skip hard exercise, alcohol, heat, and more with easy tips. You get facts on food, meds, and habits from trusted sources. At EIRMED, we support with safe items for fertility. Use this to make good choices, feel less worry, and stay healthy during the wait. Knowledge makes the path clearer.
The main activities to avoid are those that can cause physical stress or increase the risk of infection.
Yes, you should strictly avoid or significantly limit all three.
You should avoid non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and Naproxen (Aleve) unless specifically instructed by your fertility doctor. These can sometimes interfere with implantation. Always consult your doctor before taking any new over-the-counter medication or supplements.
Yes, sex after IUI is generally safe and often encouraged.
Your doctor may advise against intercourse in certain situations, including:
The cost of one IUI cycle in Texas can vary widely by clinic and what is included in the “cycle package.”
In Texas, unlike some other states, there is no state law mandating insurance coverage for infertility treatment. Therefore, coverage depends entirely on your specific insurance plan.
Beyond general healthy eating, you should follow early pregnancy food safety guidelines, which are not consistently listed on IUI sites:
Yes, as a precautionary measure during the two-week wait, many doctors suggest:
There is no scientific evidence that any specific sleeping position (side, back, or stomach) increases the success of implantation after IUI. After a brief rest period at the clinic (15-30 minutes), you can sleep in whatever position is most comfortable for you. Prioritizing a good night’s sleep is more important than your physical position.
Many people confuse normal post-IUI symptoms with implantation.
| Symptom | Typical Timing | What it is most likely caused by |
| Mild Cramping/Spotting | Within 1-2 days of IUI | The procedure itself, or normal ovulation/hormone fluctuation. |
| Implantation Cramps | 6 to 12 days after IUI | Theorized to be the embryo embedding in the uterine lining. They are usually very mild, brief, and often accompanied by light spotting (“implantation bleeding”). |
This info is for learning and not doctor advice. Always talk to your health pro before changes. EIRMED products help but do not promise success. Results differ. We use open web facts, but check with experts for your case.
Thank you for reading about things to avoid after IUI. We hope these tips make your wait easier and bring good news. At EIRMED, we are here with products for your needs. Take care and stay hopeful.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
Stages of adenomyosis refer to how deep the problem grows in your uterus wall. This condition happens when the lining of your uterus starts to grow into the muscle layer. It can cause pain and other issues. Many women learn about it when they have trouble with periods or trying to have a baby. In this article, we will look at what adenomyosis is, why it happens, and the four main stages. We draw from trusted health sites and fertility centers to give you clear facts. You will also find tips on how it links to fertility and what you can do.
Adenomyosis is a health issue where the inner lining of your uterus pushes into the outer muscle part. This makes your uterus bigger and can lead to discomfort. It is different from endometriosis, where the lining grows outside the uterus. Here, it stays inside but in the wrong spot.

Doctors think it affects about one in five women, but many do not know they have it. It often shows up in women over 30 who have had kids. The extra tissue acts like normal lining during your period, causing swelling and pain.
This can make everyday tasks hard. But with the right info, you can handle it better. At EIRMED, we help women with such issues through our fertility products.
No one knows the exact cause of adenomyosis. Some experts say it might start from childbirth. During a C-section or normal birth, the uterus wall can get small cuts, letting the lining grow in.
High estrogen levels play a role too. This hormone makes the lining thick each month. If it is too high, it can push the tissue deeper. Other ideas include stem cells in the uterus going wrong or swelling from past infections.
Age and having many periods over time might add to it. Women who start periods early or have them longer face higher risk. Knowing these helps you talk to your doctor about your own case.
You might notice signs that point to adenomyosis. Heavy bleeding during periods is a big one. Your pads or tampons fill up fast, and it lasts longer than a week.
Strong cramps in your lower belly can feel like bad period pain but worse. Some feel full or bloated all the time. Pain during sex or when using the bathroom happens too.
Tiredness from losing blood is common. If these sound like you, keep track and see a doctor. Early catch can make a difference.
Adenomyosis can make it harder to get pregnant. The swollen uterus might not let a baby implant well. It can cause early loss of pregnancy or other issues.

For women trying to have a family, this adds stress. The pain and heavy flows can make timing hard. But many still have babies with help.
At EIRMED, our products for female fertility aim to support your body. Things like supplements can help balance hormones linked to this.
To find out if you have adenomyosis, doctors start with your story. They ask about pain and periods. Then, a pelvic exam checks for a big uterus.
Ultrasound uses sound waves to see inside. It shows if the wall is thick or has spots. MRI gives clearer pictures and helps see the stages of adenomyosis.
Sometimes, a small sample from the uterus is taken. This confirms it. New ways like 3D scans make it easier to spot early.
Adenomyosis is simply when the lining of the uterus starts growing into the muscle wall of the uterus. Think of it like a weed spreading into the soil. As the “weeds” spread deeper, the symptoms usually get worse.
There’s no single, official “staging system” (like cancer has), but doctors often use a four-level idea to talk about how widespread the disease is and how bad the symptoms are.
While not a formal staging, many clinicians use a simplified four-stage model to help patients understand the progression of tissue infiltration and the associated symptom severity. This model links the depth of the disease with increasing discomfort and potential complications.
| Stage | Description of Tissue Infiltration | Key Symptoms and Impact |
| Stage 1: Early/Minimal | Minimal infiltration of endometrial tissue into the uterine wall. Infiltration is shallow. | Symptoms are often mild or non-existent (asymptomatic). May include slightly heavier-than-usual periods or occasional mild cramps. Diagnosis can be challenging at this stage. |
| Stage 2: Moderate | More pronounced infiltration affecting a larger portion of the uterine tissues. The depth of invasion is deeper. | Symptoms become more noticeable. This includes heavier periods, increased menstrual pain (dysmenorrhea), and a feeling of abdominal fullness or bloating. Pain during intercourse (dyspareunia) may also begin. |
| Stage 3: Severe | Severe and extensive infiltration, potentially distorting the normal shape of the uterus. The uterus may begin to visibly enlarge. | Symptoms intensify significantly. You may experience a serious increase in menstrual flow, debilitating cramps, and chronic pelvic pain that interferes with daily life. Fertility challenges may become more apparent. |
| Stage 4: Advanced | Extreme and deep infiltration involving a significant or even the whole area of the uterus. This often results in a greatly enlarged uterus. | Symptoms are chronic and severe. This stage is characterized by persistent, debilitating pelvic pain, very heavy and prolonged bleeding, and a high risk of complications like anemia and infertility. Surgical intervention, such as a hysterectomy, is often considered. |
Another common way doctors classify adenomyosis is by the pattern and location of the lesions within the muscular uterine wall, often determined through imaging like Transvaginal Ultrasound (TVUS) and MRI. This classification is vital for planning organ-sparing surgical procedures.
More granular classifications use the depth of invasion relative to the uterine layers, which is crucial for surgical and fertility planning:
Do not wait if signs get worse. Early help is best.
This change brings relief for many.
Fertility centers share fresh info.
Tests tell them apart.
Here is one excellent, detailed video that explains adenomyosis, covering the progression of the disease and its management, which directly relates to understanding its different “stages.”
Title: Adenomyosis EXPLAINED: Symptoms You Can’t Ignore + Treatment Options
This guide on stages of adenomyosis helps you understand the condition in easy steps. It covers causes, signs, and each stage from early to advanced. You learn how it affects fertility and ways to manage it. With tips on diagnosis and treatments, you can make smart choices. At EIRMED, we support your health with products. Stay informed and talk to doctors for best care. Knowledge gives you power to feel better.
A: No, not in the same way. Adenomyosis does not have a single, universal, or officially adopted staging system (like a Stage 1-4) that all doctors use. The term “stages” often refers to the progression of the disease’s severity and the depth of tissue infiltration, which is categorized by imaging and symptom severity. Doctors use different classification systems based on the disease’s location (focal vs. diffuse) and depth (inner or outer myometrium) to guide treatment.
A: While unofficial, these stages are typically used to describe the severity of symptoms and tissue invasion:
A: This classification is based on where the abnormal tissue is located and is crucial for diagnosis via MRI or ultrasound:
A: Scientifically, adenomyosis is often classified by the layer of muscle (myometrium) affected:
A: Not always, but often. Adenomyosis is generally considered a progressive disease, meaning symptoms often worsen over time until menopause, when the condition typically resolves because it is hormone-dependent. However, the rate of progression varies greatly among women. For some, it may remain mild for years.
A: Yes. Up to one-third of women with adenomyosis are asymptomatic (have no symptoms) despite having significant tissue infiltration detected on imaging. Conversely, some women with mild infiltration experience debilitating pain. Symptoms do not always correlate perfectly with the extent or ‘stage’ of the disease.
A: The main complications are:
A: Severity is determined by a combination of factors:
A: There is no known cure besides a hysterectomy (removal of the uterus). However, treatments focus on managing and suppressing the symptoms, which effectively halts the progression and reduces the perceived severity or ‘stage’ for the patient. Treatments include hormonal therapies (like progestin IUDs) and medications to control pain and bleeding.
This article is for general knowledge only and not medical advice. Always see a healthcare provider for your symptoms or treatments. EIRMED products aid health but do not cure. Results can differ. We use info from public sources, but check with pros for your needs.
Thank you for taking time to read about the stages of adenomyosis. We hope this info makes things clearer for you. At EIRMED, we care about your health and fertility. If you have questions, reach out. Take care and stay strong.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.
How to treat hormonal imbalance to get pregnant naturally is a common worry for many women who dream of starting a family. Your hormones play a big part in your body’s work, like controlling your monthly cycle and helping you ovulate. When they are out of balance, it can make it hard to conceive. But the good news is, you can make changes in your daily life to fix this. In this article, we will look at what causes this problem, signs to watch for, and natural steps to help you get back on track. We draw from trusted sources and what other fertility sites share to give you the best tips.
Hormones are like messengers in your body. They tell your organs what to do. For women, key hormones like estrogen, progesterone, and thyroid hormones help with ovulation and preparing your womb for a baby. When these are not in balance, it can stop you from releasing an egg each month or make your cycle irregular.
This imbalance can come from many things. For example, stress from work or life can raise cortisol, a hormone that throws off others. Being too heavy or too thin can also change how your body makes hormones. Conditions like PCOS, where cysts grow on ovaries, often cause high levels of male hormones and make periods skip. If you have thyroid issues, it might slow down your metabolism and affect fertility too.
Why does this matter for getting pregnant? Balanced hormones help your eggs grow well and your uterus get ready for implantation. Without balance, you might not ovulate, or the egg quality could be low. But many women find ways to fix this naturally before needing doctor help.
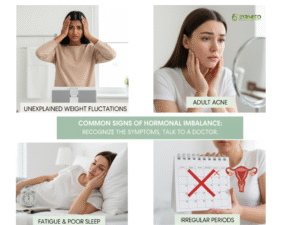 You may not know your hormones are off until you try to get pregnant. Look for these common signs. Irregular periods are a big clue – maybe they come too often or skip months. You could feel very tired all the time, even after sleep. Mood swings, like feeling sad or angry for no reason, happen too.
You may not know your hormones are off until you try to get pregnant. Look for these common signs. Irregular periods are a big clue – maybe they come too often or skip months. You could feel very tired all the time, even after sleep. Mood swings, like feeling sad or angry for no reason, happen too.
Common signs of Hormonal Imbalance include:
Irregular or missed periods: Cycles that are inconsistent often indicate problems with ovulation.
Sudden weight gain or difficulty losing weight: Hormones regulate metabolism; imbalances can lead to stubborn fat storage.
Acne or oily skin: Excess androgens can increase oil production and cause breakouts.
Thinning hair or hair loss: Often linked to thyroid disorders or high androgen levels.
Mood swings and depression: Hormonal changes affect serotonin and stress levels.
Fatigue and poor sleep: Low thyroid or progesterone levels may reduce energy.
Low libido or vaginal dryness: Reduced estrogen or testosterone can impact sexual health.
Hot flashes or night sweats: Indicate unstable estrogen levels.
Other signs include weight gain that won’t go away, acne on your face, or extra hair growth where you don’t want it. Trouble sleeping or low sex drive can point to this problem as well. If you notice these, talk to your doctor. But remember, simple changes can help a lot.
Many things can cause your hormones to go out of balance. Stress is a top one – it makes your body produce too much cortisol, which blocks other hormones. Poor diet, like eating too much sugar or processed foods, can lead to insulin issues and affect your cycle.
Major causes of hormonal imbalance include:
Polycystic Ovary Syndrome (PCOS): A condition that increases androgen levels and prevents regular ovulation.
Thyroid disorders: Both underactive and overactive thyroid glands affect reproductive hormones.
High stress levels: Chronic stress raises cortisol, which can suppress reproductive hormones.
Unhealthy diet: Nutrient deficiencies or processed foods can disturb hormone regulation.
Excessive exercise or low body weight: These reduce estrogen and stop ovulation.
Environmental toxins: Chemicals like BPA and pesticides can mimic or block natural hormones.
Aging: After age 35, natural hormonal shifts can reduce fertility.
Certain medications: Some drugs interfere with the body’s hormone production.
Not getting enough sleep messes with melatonin and other hormones. Exposure to chemicals in plastics or beauty products can act like fake hormones in your body. Age plays a role too – as you get older, hormone levels change naturally. Medical issues like diabetes or thyroid problems add to it. Knowing the cause helps you choose the right fixes.
One of the best ways to treat hormonal imbalance to get pregnant naturally is by changing what you eat. Food gives your body the building blocks for hormones. Focus on whole foods like fruits, vegetables, and lean proteins. A Mediterranean diet works well – it includes olive oil, fish, nuts, and greens. This helps lower inflammation and balance blood sugar.
Eat more fiber from beans and whole grains to help remove extra estrogen. Cut down on sugar and white bread to keep insulin steady. Add healthy fats from avocados and seeds – they support hormone making. Drink plenty of water and try herbal teas like spearmint for PCOS.
Here is a simple table of foods to include and avoid:
| Foods to Eat | Why They Help | Foods to Avoid | Why They Harm |
|---|---|---|---|
| Salmon | Rich in omega-3 for hormone balance | Sugary drinks | Raise insulin and disrupt cycles |
| Broccoli | Helps detox extra hormones | Fried foods | Add bad fats that cause inflammation |
| Eggs | Provide protein for egg health | Processed meats | Have chemicals that mimic hormones |
| Berries | Antioxidants protect cells | Caffeine excess | Can stress your adrenal glands |
At EIRMED, we have natural supplements with these nutrients to make it easier for you.
Moving your body helps balance hormones. Aim for moderate exercise like walking or swimming, 30 minutes most days. This lowers stress and helps with weight, which affects hormones. Yoga is great – it calms your mind and boosts blood flow to your reproductive organs.
Avoid hard workouts that tire you out too much, as they can raise cortisol. Strength training with light weights builds muscle and helps insulin work better. Listen to your body – if you feel good after exercise, it’s helping your fertility.
Good sleep fixes many hormone issues. Your body repairs during rest. Lack of sleep raises cortisol and lowers melatonin, which affects fertility. Make a bedtime routine – no screens an hour before bed.
Keep your room cool and dark. If you wake up often, try relaxing teas. Better sleep means better hormone balance and higher chances to conceive.
Yes, hormone levels naturally change with age, and this can significantly influence fertility. As a woman grows older, her ovaries gradually produce fewer eggs and lower amounts of estrogen, progesterone, and other reproductive hormones. This shift typically begins in the early 30s and becomes more noticeable after 35. Reduced hormone levels can make ovulation less regular and decrease egg quality, making it more difficult to conceive naturally.
Here’s how age impacts hormone levels and fertility:
Decreased estrogen and progesterone: These hormones decline with age, leading to irregular menstrual cycles and weaker uterine lining preparation.
Reduced FSH sensitivity: The ovaries become less responsive to Follicle-Stimulating Hormone (FSH), causing slower egg development.
Fewer viable eggs: The number of eggs (ovarian reserve) decreases over time, limiting chances of conception.
Higher risk of hormonal fluctuations: Hormone patterns become inconsistent, sometimes leading to missed or shorter periods.
Increased chance of early perimenopause: Some women experience hormone-related changes earlier due to genetics or lifestyle.
Maintaining a healthy lifestyle, managing stress, and following a balanced diet can help support hormonal health as a woman ages.
(Sources for your better knowledge: NHS, Cleveland Clinic, PubMed Central)
Changes in menstrual patterns can sometimes be early signs of perimenopause, the transition phase before menopause. During this time, the ovaries gradually produce less estrogen and progesterone, which leads to irregular cycles and other symptoms. While occasional irregular periods can also result from stress or thyroid imbalance, persistent cycle changes after age 40 often signal the beginning of perimenopause.
Common signs that may indicate early menopause or perimenopause include:
Irregular or skipped periods: Cycles may become shorter, longer, or unpredictable.
Hot flashes and night sweats: Sudden feelings of heat due to fluctuating estrogen levels.
Sleep problems: Hormonal changes can cause insomnia or restless nights.
Mood swings or irritability: Estrogen affects serotonin, so its decline impacts mood.
Vaginal dryness or discomfort: Lower estrogen reduces natural lubrication.
Decreased fertility: Ovulation becomes less frequent, reducing the chances of pregnancy.
If these symptoms persist, it’s best to consult a healthcare provider to confirm whether the cause is perimenopause or another hormonal imbalance.
(Sources for your better knowledge: Mayo Clinic)
 Yes, it is important to address hormonal imbalances even if pregnancy is not a current goal. Hormones regulate far more than fertility—they influence mood, metabolism, heart health, bone strength, and cognitive function. Leaving a hormonal imbalance untreated can increase the risk of long-term health issues such as thyroid disease, osteoporosis, or metabolic disorders.
Yes, it is important to address hormonal imbalances even if pregnancy is not a current goal. Hormones regulate far more than fertility—they influence mood, metabolism, heart health, bone strength, and cognitive function. Leaving a hormonal imbalance untreated can increase the risk of long-term health issues such as thyroid disease, osteoporosis, or metabolic disorders.
Reasons to seek medical help for hormonal imbalance include:
Persistent irregular periods: Could indicate thyroid or ovarian disorders.
Unexplained weight changes: Often linked to hormonal or metabolic dysfunction.
Severe acne or excessive hair growth: May signal excess androgen production.
Chronic fatigue or mood swings: Can result from thyroid or adrenal imbalances.
Early signs of menopause: Medical advice can ease symptoms and protect long-term health.
Family history of hormonal disorders: Regular checkups help in early detection and management.
Getting blood tests and professional evaluations ensures early diagnosis and helps maintain hormonal balance throughout life.
(Sources for your better knowledge: Cleveland Clinic)
Treating hormonal imbalance while trying to conceive focuses on restoring the natural rhythm of ovulation and supporting overall reproductive health. The treatment depends on the underlying cause—whether it’s PCOS, thyroid disorder, stress, or poor nutrition. Many women benefit from combining lifestyle changes with medical treatments that help regulate hormone levels and promote natural conception.
Common treatment and management approaches include:
Lifestyle modifications: A balanced diet, adequate sleep, and regular exercise can naturally improve hormone regulation.
Stress management: Techniques like yoga, deep breathing, or meditation reduce cortisol levels that interfere with ovulation.
Balanced diet: Include zinc, iron, healthy fats, and vitamins (especially B-complex and D) to support reproductive hormones.
Medical treatments: Doctors may prescribe medications such as clomiPHENE citrate (Clomid) to trigger ovulation or metFORMIN to manage insulin resistance in PCOS.
Thyroid and prolactin correction: If imbalances exist, medication can restore normal levels and improve fertility chances.
Herbal or natural supplements: Some women use supplements like Vitex (Chasteberry) under medical guidance to regulate menstrual cycles.
Maintaining healthy body weight: Both underweight and overweight conditions disturb estrogen and progesterone balance.
With proper diagnosis and consistent management, many women successfully restore hormonal balance and conceive naturally or with minimal medical assistance.
(Sources for your better knowledge: Mayo Clinic, Cleveland Clinic)
Jennifer, a 30-year-old wellness blogger and occupational therapist, struggled with infertility for about 2.5 years. She discovered through hormone testing that she had a hormonal imbalance, which was partly due to overexercising and under-eating (which disrupted her menstrual cycle). After consulting her doctor, she followed a treatment plan involving supplements, lifestyle adjustments, and medical oversight. Eventually, she conceived her first child. For her second pregnancy, having better knowledge of her body and hormones made conception quicker.
Key takeaways:
• Hormone testing helped identify hidden imbalances
• Tailored treatment (diet, stress, supplements) can help restore fertility
• Understanding your body helps speed future conception
Julie, 32, had a history of heavy, painful periods, PMS, endometriosis, and had tried three rounds of IVF without success. She also had Hashimoto’s (thyroid autoimmune disorder). In functional medicine evaluation, the practitioner addressed not just hormones but also diet, inflammation, thyroid support, gut health, and lifestyle. The holistic approach helped rebalance her hormones, relieve symptoms, and improve her fertility outlook.
Key takeaways:
• Addressing coexisting conditions (like thyroid) is critical
• Diet, inflammation control, and systemic support matter, not just reproductive hormones
• A broader approach can complement conventional fertility treatments
Diana struggled with PCOS for years without regular monthly cycles. She used natural progesterone cream (topically), improved her nutrition (including vitamin D), and followed fertility-supportive suggestions (herbal and lifestyle adjustments). Soon after implementing those changes, she became pregnant naturally.
Key lessons:
• Natural progesterone in some cases can help restart cycles
• Addressing lifestyle, diet, and nutrient deficiencies matters
• Success sometimes follows persistent, stepped efforts
In this video, Dr. Uthuman discusses how hormonal imbalances can lead to infertility and shares ways to identify symptoms of hormonal problems. She explains common hormone issues that affect fertility (like irregular cycles, progesterone insufficiency, thyroid or androgen problems) and offers strategies to correct those imbalances naturally and medically—such as nutrition, lifestyle changes, and targeted therapies.
Video Title: HOW TO GET PREGNANT WITH HORMONAL IMBALANCE
Irregular periods often mean your hormones like estrogen and progesterone are off, which can stop ovulation. To help naturally, start with a balanced diet full of veggies, fruits, and healthy fats like nuts and fish. These foods support your body’s hormone making. Exercise gently, like walking or yoga, to lower stress and keep your weight steady. Aim for 7-9 hours of sleep each night, as poor rest raises cortisol, a stress hormone that throws off others. Track your cycle with apps to spot ovulation days. If you have PCOS, try supplements like inositol after checking with a doctor – it can help regulate insulin and cycles. Many women see better periods in 3-6 months with these changes, raising pregnancy odds.
Yes, lifestyle tweaks can help a lot. Eat foods rich in fiber, like beans and whole grains, to clear extra estrogen from your body. Cut down on sugar and processed snacks to keep blood sugar even, which aids hormone balance. Drink herbal teas like spearmint to lower male hormones if you have PCOS. Move your body with fun activities, but don’t overdo it – too much hard exercise can raise stress hormones. Manage worry with deep breaths or time in nature. Herbs like Chasteberry may help cycles, but start low and watch for side effects. Avoid plastics with chemicals that mimic hormones. These steps can boost egg quality and make conception easier over time.
Common causes include stress, which boosts cortisol and blocks ovulation hormones. Poor eating, like too much junk food, can mess with insulin and lead to weight gain, worsening the issue. Conditions like PCOS cause high androgens, making periods skip. Thyroid problems slow your body and affect egg release. Not enough sleep or exposure to toxins in products can act like fake hormones. As you age, levels drop naturally. Fixing the root, like better diet or less stress, often helps restore balance for better fertility.
Hormonal imbalances can stop you from ovulating or make your womb lining thin, leading to infertility. For natural fixes, focus on weight – being too heavy or thin affects hormones. Lose or gain slowly with whole foods and movement. Take vitamins like B6 for progesterone support and D for overall hormone health. Practice yoga to improve blood flow to your ovaries. Limit caffeine and alcohol, as they stress your adrenals. If it’s PCOS-related, Maca root might help balance, but talk to a pro first. Many women conceive after 3 months of these habits.
For PCOS, cut carbs to manage insulin, which often causes hormone spikes. Eat anti-inflammatory foods like salmon for omega-3s to calm your system. Try acupuncture – it may regulate cycles by boosting blood flow. Supplements like magnesium and zinc support progesterone, key for pregnancy. Track fertile days with kits. Reduce stress with meditation, as it lowers androgens. Avoid dairy if it worsens symptoms. These can help ovulate more often, upping your chances.
Low progesterone can make it hard for a baby to stick. Boost it with seeds like sesame in the second half of your cycle. Take vitamin C-rich foods like berries to support your adrenals. Avoid over-exercising; choose gentle walks. Herbs like Vitex (Chasteberry) can raise progesterone over time. Get good sleep in a dark room. If needed, add a B-complex vitamin. These steps help your body hold a pregnancy better.
Eat cruciferous veggies like broccoli to detox extra hormones. Add avocados for healthy fats that build hormones. Berries fight inflammation. Whole grains keep blood sugar steady. Nuts and seeds provide zinc for ovulation. Avoid fried foods and sugar. A Mediterranean-style diet works best for fertility. Drink water and green tea. These choices can balance hormones in weeks.
Inositol for insulin control in PCOS. CoQ10 for egg health. Omega-3s from fish oil reduce swelling. Vitamin D if you’re low – it aids hormone work. Maca root for overall balance. Always check doses with a doctor, as too much can harm. Start slow and track changes.
It often takes 3-6 months with steady changes like diet and exercise. Your body needs time to adjust. Track symptoms and cycles. If no improvement, see a fertility doctor for tests.
If you’ve tried for 6-12 months without luck, get checked. Tests can spot issues like thyroid or PCOS. Natural ways help many, but some need extra support like meds to ovulate. Early help raises success rates.
The purpose of this article is to educate women about how hormonal balance directly affects fertility and natural conception. It explains the key hormones involved in reproduction, the common signs and causes of hormonal imbalance, and how these imbalances can interfere with ovulation, egg quality, and menstrual cycles.
The article also highlights how age impacts hormone levels, how menstrual changes may signal perimenopause, and why it’s important to seek medical help for hormonal issues even outside pregnancy planning. Finally, it provides insights into effective treatments and natural methods to restore hormone balance, helping women improve their chances of getting pregnant naturally and maintain long-term reproductive health.
This content is for information only and not medical advice. Always see a doctor before changing your diet, exercise, or taking supplements. EIRMED products are to support health, but results vary. We do not promise cures. Talk to your healthcare provider about your fertility concerns.
Thank you for reading this guide on how to treat hormonal imbalance to get pregnant naturally. We hope these tips help you feel more hopeful on your path to parenthood. At EIRMED, we are here to support you with quality products. Share your story with us!

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.