10 Reasons for Blocked Fallopian Tubes: Essential Insights for Your Fertility Journey
 Reasons for blocked tubes can be a confusing and emotional topic if you’re facing fertility challenges. These tubes play a key role in getting pregnant, acting as the path where eggs and sperm meet. If they’re blocked, it might stop that from happening naturally. At EIRMED, we focus on helping you understand these issues so you can make smart choices about your health. Let’s explore the common causes, signs, and ways to handle them, all in a way that’s easy to follow and supportive.
Reasons for blocked tubes can be a confusing and emotional topic if you’re facing fertility challenges. These tubes play a key role in getting pregnant, acting as the path where eggs and sperm meet. If they’re blocked, it might stop that from happening naturally. At EIRMED, we focus on helping you understand these issues so you can make smart choices about your health. Let’s explore the common causes, signs, and ways to handle them, all in a way that’s easy to follow and supportive.What Are Fallopian Tubes and Their Role in Fertility?
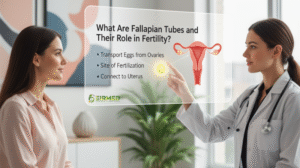 Fallopian tubes are slim passages linking your ovaries to your uterus. Each month, an egg moves through them, hoping to meet sperm for fertilization. When things go right, the fertilized egg travels to the uterus to grow into a baby. But if there’s a blockage, it can lead to infertility. Understanding fallopian tube problems is crucial because they affect about 25-30% of infertility cases in women, based on insights from fertility experts like those at the Cleveland Clinic and Healthline.
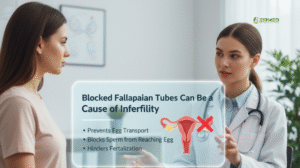
Fallopian tubes are slim passages linking your ovaries to your uterus. Each month, an egg moves through them, hoping to meet sperm for fertilization. When things go right, the fertilized egg travels to the uterus to grow into a baby. But if there’s a blockage, it can lead to infertility. Understanding fallopian tube problems is crucial because they affect about 25-30% of infertility cases in women, based on insights from fertility experts like those at the Cleveland Clinic and Healthline.Blocked Fallopian Tubes Can Be a Cause of Infertility
Yes, blocked fallopian tubes can be a cause of infertility, preventing sperm from reaching the egg or the embryo from getting to the uterus. This is often called tubal factor infertility. Sources from Mayo Clinic and WebMD note that without clear tubes, natural conception becomes tough, but options like IVF can bypass this issue entirely.
Causes of Blocked Fallopian Tubes
| Location of Blockage | Typical Causes |
|---|---|
| Proximal (near uterus) | Tubal spasm, scarring from inflammation, debris, or small growths (polyps) in the tube (Veritas Fertility & Surgery) |
| Mid-segment (middle of tube) | Previous tubal ligation (surgical “tying” of tubes), history of ectopic (tubal) pregnancy, pelvic adhesions (scar tissue), endometriosis (Veritas Fertility & Surgery) |
| Distal / Hydrosalpinx (far end toward ovary) | Past pelvic infections (PID), severe endometriosis, tuberculosis in some regions (Veritas Fertility & Surgery) |
What are the symptoms of tubal blockage? | What Cause Fallopian Tube Blockage?
In most cases, tubal blockage doesn’t show obvious symptoms. Many women don’t even realize their fallopian tubes are blocked until they face trouble getting pregnant. The condition is often discovered during fertility checkups.
However, some women may notice signs depending on the cause of the blockage:
-
Infertility – The most common “symptom.” If a woman is trying to conceive for a long time without success, blocked tubes may be a reason.
-
Pelvic pain – If the blockage is linked to endometriosis or pelvic inflammatory disease (PID), ongoing pain in the lower belly or pelvis may occur.
-
Painful or irregular periods – Conditions like endometriosis may cause heavy, painful, or irregular menstrual cycles.
-
Unusual vaginal discharge – Infections such as PID can sometimes cause abnormal discharge, which may signal tubal damage.
-
Risk of ectopic pregnancy – If the tube is partially blocked, a fertilized egg may get stuck in the tube instead of reaching the uterus, leading to an ectopic pregnancy. This can cause severe pain, vaginal bleeding, and is a medical emergency.
Reasons For Blocked Fallopian Tubes
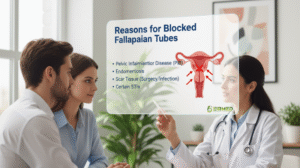 Diving deeper, reasons for blocked fallopian tubes include past infections beyond PID, like those from miscarriages or abortions. Scar tissue from pelvic surgeries or conditions such as irritable bowel syndrome can compress the tubes. Congenital issues, where tubes are abnormal from birth, are rare but possible. Unexplained blockages happen, too, frustrating many women. Competitor insights from Illume Fertility and PFCLA emphasize that STIs and endometriosis are frequent culprits, urging regular check-ups to catch problems early.
Diving deeper, reasons for blocked fallopian tubes include past infections beyond PID, like those from miscarriages or abortions. Scar tissue from pelvic surgeries or conditions such as irritable bowel syndrome can compress the tubes. Congenital issues, where tubes are abnormal from birth, are rare but possible. Unexplained blockages happen, too, frustrating many women. Competitor insights from Illume Fertility and PFCLA emphasize that STIs and endometriosis are frequent culprits, urging regular check-ups to catch problems early.Reason 1: Pelvic Infections (PID)
Reason 2: Endometriosis
Reason 3: Past Surgeries
Reason 4: Sexually Transmitted Infections (STIs)
Reason 5: Fibroids in the Uterus
Reason 6: Hydrosalpinx (Fluid in Tubes)
Reason 7: Tuberculosis in the Pelvis
Reason 8: Ectopic Pregnancy
Reason 9: Birth Problems with Tubes
Reason 10: Scar Tissue (Adhesions)
Scarred Fallopian Tubes: How Scarring Develops
What Causes Fallopian Tube Blockage?
Fallopian Tube Issues: Common Problems Explained
Fallopian Tube Damage: Signs and Impacts
Fallopian tube damage might show as pelvic pain, especially during periods or sex, or irregular cycles. However, many women experience no signs until they attempt to conceive. Damage from infections or surgeries can lead to infertility or ectopics. PFCLA and Positive Steps Fertility highlight that scarring reduces the flexibility of the fallopian tubes, making it difficult for eggs to be transported.
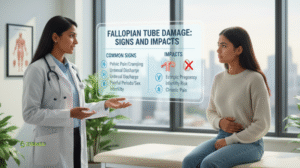
Fallopian tube damage often goes unnoticed because it may not cause any obvious symptoms. The most common sign is often difficulty conceiving. However, in some cases, there can be other symptoms and serious health impacts.
Signs of Fallopian Tube Damage
Many women with damaged or blocked fallopian tubes are asymptomatic and only discover the issue when they have trouble getting pregnant. However, some women may experience the following:
- Pelvic or Abdominal Pain: This pain can range from mild to severe and may be constant or occur at specific times, such as during menstruation.
- Painful Menstruation (Dysmenorrhea): Pressure and fluid accumulation behind a blocked tube can lead to discomfort during your period.
- Abnormal Vaginal Discharge: Obstruction of the fallopian tubes can alter fluid dynamics in the reproductive system, leading to unusual discharge.
- Painful Intercourse or Urination: Inflammation or obstruction can affect sexual activity and urination.
- Symptoms of Underlying Conditions: Fallopian tube damage is often caused by other conditions, and you may experience the symptoms of those conditions, such as:
- Endometriosis: Severe pelvic pain and heavy or irregular periods.
- Pelvic Inflammatory Disease (PID): Lower abdominal pain, fever, and abnormal vaginal discharge.
- Hydrosalpinx: A specific type of blockage where fluid fills and enlarges the fallopian tube, which can cause mild, consistent pain on one side of the abdomen.
Impacts on Fertility and Health
The fallopian tubes are a crucial part of the reproductive process. They are where the sperm and egg meet for fertilization and where the fertilized egg travels to the uterus for implantation. Damage to these tubes can severely impact a woman’s ability to get pregnant.
- Infertility: This is the most common impact. If the fallopian tubes are completely blocked, sperm cannot reach the egg, and a fertilized egg cannot reach the uterus.
- Ectopic Pregnancy: If a fallopian tube is only partially blocked or damaged, a fertilized egg might get stuck and implant itself in the tube instead of the uterus. This is a life-threatening medical emergency and can cause the tube to rupture, leading to severe internal bleeding. Symptoms of a ruptured ectopic pregnancy include sudden, sharp abdominal pain, fainting, and low blood pressure.
- Increased Risk of Miscarriage: A hydrosalpinx (a fluid-filled fallopian tube) can increase the risk of miscarriage even with in vitro fertilization (IVF). The fluid from the damaged tube can leak back into the uterus, making it a hostile environment for a developing embryo.
Common Causes of Fallopian Tube Damage
Damage to the fallopian tubes is most often caused by the formation of scar tissue. The most frequent causes include:
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs, often caused by untreated sexually transmitted infections (STIs) like chlamydia and gonorrhea.
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, which can lead to inflammation and scarring in the tubes.
- Previous Abdominal or Pelvic Surgery: Surgeries, especially those on the fallopian tubes themselves, can cause adhesions (bands of scar tissue) that block the tubes.
- Past Ectopic Pregnancy: An ectopic pregnancy can cause scarring and damage to the fallopian tube.
- Uterine Fibroids: These non-cancerous growths can sometimes block the fallopian tubes.
Closed Fallopian Tubes: What It Means for You
 Closed fallopian tubes mean complete blockage, often from severe scarring or hydrosalpinx. This fully stops natural conception on that side. If both are closed, IVF becomes key. Insights from CNY Fertility explain that closure traps fluid, harming embryo implantation even in IVF, so removal might be needed.
Closed fallopian tubes mean complete blockage, often from severe scarring or hydrosalpinx. This fully stops natural conception on that side. If both are closed, IVF becomes key. Insights from CNY Fertility explain that closure traps fluid, harming embryo implantation even in IVF, so removal might be needed.How to Know If Your Fallopian Tubes Are Blocked
Treatment for Blocked Fallopian Tubes
Cure for Blocked Fallopian Tubes
Cure Blocked Fallopian Tubes Naturally
Natural Fertility Therapy for Blocked Tubes
Signs of Blocked Tubes
- Trouble getting pregnant for more than a year
- Pain during sex or periods
- Lower belly or pelvic pain
- Unusual vaginal discharge
- Often, no clear symptoms at all
Tests to Check Blocked Tubes
- HSG (Hysterosalpingography): X-ray with dye to see if tubes are open
- Sonohysterography: Ultrasound with special fluid
- Laparoscopy: Small surgery to check directly
Prevention Tips for Healthy Fallopian Tubes
 To avoid blockages, treat STIs promptly, use protection, and undergo regular gynecological exams. Avoid smoking, which harms reproductive health. Maintain a healthy weight to reduce your risk of endometriosis. Insights from Medical News Today suggest that lifestyle changes can lower the chances of infection, protecting tubes in the long term.
To avoid blockages, treat STIs promptly, use protection, and undergo regular gynecological exams. Avoid smoking, which harms reproductive health. Maintain a healthy weight to reduce your risk of endometriosis. Insights from Medical News Today suggest that lifestyle changes can lower the chances of infection, protecting tubes in the long term.- Get regular STI checkups.
- Use protection during sex.
- Treat infections quickly
- Eat healthy food and stay active.
- Avoid smoking and heavy drinking.
Overall Purpose
Thank You
FAQs
What Causes Blocked Fallopian Tubes?
Blocked fallopian tubes often result from pelvic inflammatory disease (PID) due to untreated infections like chlamydia or gonorrhea, causing scarring. Endometriosis, pelvic surgeries, ectopic pregnancies, or tubal ligation also contribute. Why might early treatment of infections prevent this? Regular check-ups catch issues before scarring occurs.
What Are the Symptoms of Blocked Fallopian Tubes?
Most women have no symptoms, discovering blockages during fertility tests. Some experience pelvic pain, painful periods, or discomfort during sex if caused by endometriosis or PID. Why do silent conditions like this go unnoticed? Routine screenings can reveal issues early.
How Do Blocked Fallopian Tubes Affect Fertility?
Blockages prevent egg and sperm from meeting, causing infertility in about 25% of cases. Partial blockages may allow pregnancy but raise ectopic pregnancy risks. Why does the blockage’s location matter? Proximal blockages (near the uterus) have better outcomes.
How Are Blocked Fallopian Tubes Diagnosed?
A hysterosalpingogram (HSG) uses dye and X-rays to check tube patency non-invasively. Ultrasound or laparoscopy may confirm findings. Why opt for non-surgical tests first? They’re less invasive and often sufficient for diagnosis.
What Are the Treatments for Blocked Fallopian Tubes?
Laparoscopic surgery can clear minor blockages or reconnect tubes. For severe cases, IVF bypasses the tubes. Why consult a specialist? Tailored plans based on blockage type improve success.
Can You Get Pregnant with One Blocked Fallopian Tube?
Yes, pregnancy is possible if one tube is open, as ovaries alternate ovulation. Success depends on the open tube’s health. Why track ovulation? It boosts chances by timing conception.
Can Blocked Fallopian Tubes Be Unblocked Naturally?
No reliable natural remedies unblock tubes. Herbs or massages lack evidence and may delay care. Why prioritize medical advice? Proven treatments like surgery or IVF offer better outcomes.
Disclaimer

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.


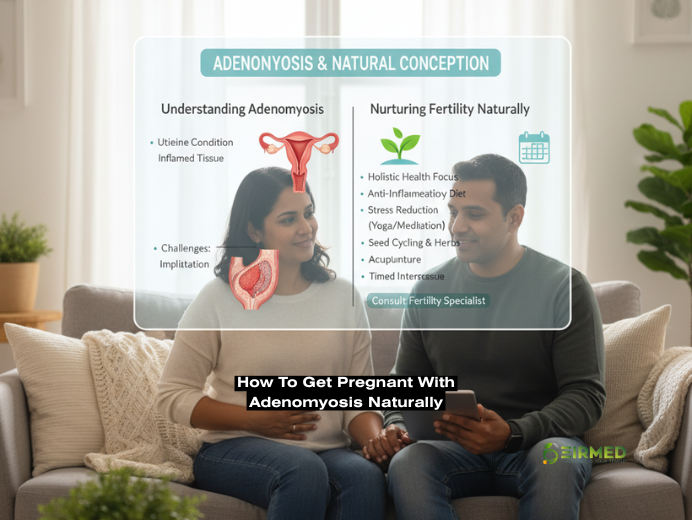
 How to get pregnant with adenomyosis naturally is a question many women ask when facing this common yet challenging condition. It involves the inner lining of the uterus growing into its muscular wall, leading to discomfort that can disrupt daily life and dreams of starting a family. But you are not alone in this; countless women have found ways to support their bodies and achieve pregnancy through gentle, everyday adjustments.
How to get pregnant with adenomyosis naturally is a question many women ask when facing this common yet challenging condition. It involves the inner lining of the uterus growing into its muscular wall, leading to discomfort that can disrupt daily life and dreams of starting a family. But you are not alone in this; countless women have found ways to support their bodies and achieve pregnancy through gentle, everyday adjustments. Adenomyosis occurs when endometrial tissue, which should only line the uterus, invades the muscle layer, causing the uterus to enlarge and become tender. This can lead to heavier periods and ongoing discomfort, affecting about one in ten women, often in their 30s or 40s. Based on information from reliable sources, the condition stems from factors like prior uterine surgeries or hormonal shifts, creating an environment where inflammation thrives. Unlike endometriosis, where tissue grows outside the uterus, adenomyosis stays within, but both can overlap, complicating matters. Recognizing early signs helps in planning ahead, especially if family-building is on your mind.
Adenomyosis occurs when endometrial tissue, which should only line the uterus, invades the muscle layer, causing the uterus to enlarge and become tender. This can lead to heavier periods and ongoing discomfort, affecting about one in ten women, often in their 30s or 40s. Based on information from reliable sources, the condition stems from factors like prior uterine surgeries or hormonal shifts, creating an environment where inflammation thrives. Unlike endometriosis, where tissue grows outside the uterus, adenomyosis stays within, but both can overlap, complicating matters. Recognizing early signs helps in planning ahead, especially if family-building is on your mind. Understanding the stages of adenomyosis can help you gauge its progression and seek timely support. In the early stage
Understanding the stages of adenomyosis can help you gauge its progression and seek timely support. In the early stage Yes, you can get pregnant with adenomyosis, though it may require extra patience and care. Studies indicate that while the condition can reduce implantation success by up to 30%, many women conceive naturally or with assistance. The thickened uterine wall may hinder embryo attachment, but factors such as age and symptom severity also play a role. Women who’ve shared their journeys often highlight how addressing inflammation improved their odds. If you’ve been trying for months without success, consulting a specialist can clarify your unique situation, combining natural approaches with monitoring for optimal outcomes.
Yes, you can get pregnant with adenomyosis, though it may require extra patience and care. Studies indicate that while the condition can reduce implantation success by up to 30%, many women conceive naturally or with assistance. The thickened uterine wall may hinder embryo attachment, but factors such as age and symptom severity also play a role. Women who’ve shared their journeys often highlight how addressing inflammation improved their odds. If you’ve been trying for months without success, consulting a specialist can clarify your unique situation, combining natural approaches with monitoring for optimal outcomes. How I cured my adenomyosis without surgery often involves non-invasive options like UAE or hormonal therapies, but many opt for natural routes. Women report relief through a consistent diet and acupuncture, avoiding operations while improving fertility.
How I cured my adenomyosis without surgery often involves non-invasive options like UAE or hormonal therapies, but many opt for natural routes. Women report relief through a consistent diet and acupuncture, avoiding operations while improving fertility.

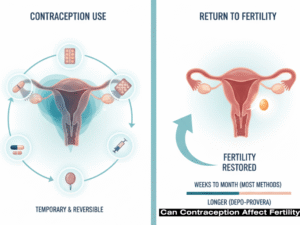 Can contraception affect fertility? This is a concern many women face when considering or stopping birth control, wondering if methods like pills or IUDs might hinder future pregnancies. The truth is, most forms of contraception are reversible and do not cause lasting infertility, allowing fertility to return soon after discontinuation. In this comprehensive guide, we’ll delve into the science behind contraception, its temporary effects on your cycle, common misconceptions, and practical steps to support your reproductive health. Drawing from trusted medical sources, we’ll address how different methods work and what you can expect when planning a family.
Can contraception affect fertility? This is a concern many women face when considering or stopping birth control, wondering if methods like pills or IUDs might hinder future pregnancies. The truth is, most forms of contraception are reversible and do not cause lasting infertility, allowing fertility to return soon after discontinuation. In this comprehensive guide, we’ll delve into the science behind contraception, its temporary effects on your cycle, common misconceptions, and practical steps to support your reproductive health. Drawing from trusted medical sources, we’ll address how different methods work and what you can expect when planning a family. Different birth control options have unique profiles, but none lead to long-term infertility. Let’s examine how each might influence your cycle after stopping.
Different birth control options have unique profiles, but none lead to long-term infertility. Let’s examine how each might influence your cycle after stopping. Depo-Provera injections provide three-month protection but can delay fertility recovery up to 18 months. Still, they do not cause permanent infertility. Implants like Nexplanon allow quicker returns, often within a month. Recovery rates reach 82.9% within a year for similar injectables.
Depo-Provera injections provide three-month protection but can delay fertility recovery up to 18 months. Still, they do not cause permanent infertility. Implants like Nexplanon allow quicker returns, often within a month. Recovery rates reach 82.9% within a year for similar injectables. Yes, short-term disruptions like irregular periods or delayed ovulation are common as hormones stabilize. This phase varies by method, with injectables taking longest. Monitoring cycles helps identify when fertility returns.
Yes, short-term disruptions like irregular periods or delayed ovulation are common as hormones stabilize. This phase varies by method, with injectables taking longest. Monitoring cycles helps identify when fertility returns. Many myths persist, but evidence shows no long-term harm. Birth control does not lead to weight gain causing infertility or damage fertility permanently. It won’t make future pregnancies harder. Misconceptions often stem from outdated fears.
Many myths persist, but evidence shows no long-term harm. Birth control does not lead to weight gain causing infertility or damage fertility permanently. It won’t make future pregnancies harder. Misconceptions often stem from outdated fears.
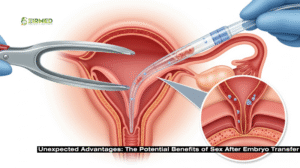 Here’s where it gets interesting: sex after embryo transfer isn’t always a no-go. Some evidence suggests it could even help. Seminal fluid packs proteins, hormones, and immune factors that signal the uterus to be more receptive. A randomized trial on FET cycles found that intercourse the night before transfer upped clinical pregnancy rates by about 24%, likely due to these immune-modulating effects. It’s like nature’s way of prepping the ground, similar to natural pregnancies where semen exposure aids implantation.
Here’s where it gets interesting: sex after embryo transfer isn’t always a no-go. Some evidence suggests it could even help. Seminal fluid packs proteins, hormones, and immune factors that signal the uterus to be more receptive. A randomized trial on FET cycles found that intercourse the night before transfer upped clinical pregnancy rates by about 24%, likely due to these immune-modulating effects. It’s like nature’s way of prepping the ground, similar to natural pregnancies where semen exposure aids implantation. Balance is key, so let’s talk risks. Orgasms trigger uterine contractions, which might dislodge an unattached embryo. One study linked intercourse during the 5-10 day implantation window to higher miscarriage odds, especially if repeated in that week. Infections pose another threat, as the transfer can breach cervical mucus, and introducing bacteria increases the chances, though rare at about 1-2%.
Balance is key, so let’s talk risks. Orgasms trigger uterine contractions, which might dislodge an unattached embryo. One study linked intercourse during the 5-10 day implantation window to higher miscarriage odds, especially if repeated in that week. Infections pose another threat, as the transfer can breach cervical mucus, and introducing bacteria increases the chances, though rare at about 1-2%. Most advice? Hold off 48 hours to 7-14 days
Most advice? Hold off 48 hours to 7-14 days  IVF strains bonds, and pausing sex after embryo transfer can amplify feelings of distance. But it’s an opportunity to nurture non-physical closeness. Research links
IVF strains bonds, and pausing sex after embryo transfer can amplify feelings of distance. But it’s an opportunity to nurture non-physical closeness. Research links 
 Signs a man is fertile can offer reassuring clues about reproductive health, especially when you’re
Signs a man is fertile can offer reassuring clues about reproductive health, especially when you’re  Male fertility involves producing enough healthy sperm to travel effectively to fertilize an egg.
Male fertility involves producing enough healthy sperm to travel effectively to fertilize an egg.  One strong sign a man is fertile is having testicles that feel normal, about the size of a walnut, firm but not hard, without pain or swelling.
One strong sign a man is fertile is having testicles that feel normal, about the size of a walnut, firm but not hard, without pain or swelling.  Balanced facial and body hair growth is another clue to hormone levels that
Balanced facial and body hair growth is another clue to hormone levels that  Look for semen that’s white or grey, about 1.5 to 5 millilitres per ejaculation, roughly a teaspoon and slightly thick at first.
Look for semen that’s white or grey, about 1.5 to 5 millilitres per ejaculation, roughly a teaspoon and slightly thick at first.  Feeling energetic throughout the day? That’s a good sign a man is fertile, linked to balanced hormones and good circulation for sperm health. Low energy might stem from poor sleep or obesity, which can cut sperm motility.
Feeling energetic throughout the day? That’s a good sign a man is fertile, linked to balanced hormones and good circulation for sperm health. Low energy might stem from poor sleep or obesity, which can cut sperm motility. A stable mood without constant stress is tied to lower cortisol, which otherwise harms sperm production. Frequent mood swings or depression could indicate hormonal shifts affecting fertility.
A stable mood without constant stress is tied to lower cortisol, which otherwise harms sperm production. Frequent mood swings or depression could indicate hormonal shifts affecting fertility. A healthy sex drive with no issues like erectile dysfunction is a direct sign that a man is fertile, showing solid blood flow and hormones. Problems here might relate to low desire or ejaculation troubles.
A healthy sex drive with no issues like erectile dysfunction is a direct sign that a man is fertile, showing solid blood flow and hormones. Problems here might relate to low desire or ejaculation troubles.
 Picture inositol as a sweet helper in your body, kind of like a sugar your cells love. It’s not a real vitamin, but people call it vitamin B8 sometimes. Your body makes it, and you get more from foods like oranges, beans, nuts, and whole grains. But if you have PCOS, which messes with hormones and sugar handling, eating enough can be hard.
Picture inositol as a sweet helper in your body, kind of like a sugar your cells love. It’s not a real vitamin, but people call it vitamin B8 sometimes. Your body makes it, and you get more from foods like oranges, beans, nuts, and whole grains. But if you have PCOS, which messes with hormones and sugar handling, eating enough can be hard. Straight up: Yes, is inositol safe during pregnancy for most women, based on what we know from studies. Groups like the Cleveland Clinic say doses up to 4 grams a day are okay short-term, with no big red flags for you or baby. One look-back at 46 moms taking it early on saw zero bad stuff compared to others who didn’t.
Straight up: Yes, is inositol safe during pregnancy for most women, based on what we know from studies. Groups like the Cleveland Clinic say doses up to 4 grams a day are okay short-term, with no big red flags for you or baby. One look-back at 46 moms taking it early on saw zero bad stuff compared to others who didn’t. Post-baby, nursing moms wonder about carry-overs. Short answer: Yep, is inositol safe during pregnancy and nursing too. It’s already in breast milk, feeding baby’s brain growth. Doses like 4 grams seem fine, maybe even upping supply.
Post-baby, nursing moms wonder about carry-overs. Short answer: Yep, is inositol safe during pregnancy and nursing too. It’s already in breast milk, feeding baby’s brain growth. Doses like 4 grams seem fine, maybe even upping supply.
 Have you ever looked at your calendar and thought, “My periods come right on time every month, does that mean I’m ready to have a baby?” Lots of people wonder about this. Are regular periods a good sign of fertility? Well, it’s a common question, and the answer isn’t always straightforward. At EIRMED, we help folks with all kinds of fertility needs, offering supplements and treatments for both guys and gals. In this piece, we’ll chat about what your menstrual cycle really tells you about getting pregnant, how it all works, and some tips to boost your chances. We’ll keep it simple so anyone can follow along.
Have you ever looked at your calendar and thought, “My periods come right on time every month, does that mean I’m ready to have a baby?” Lots of people wonder about this. Are regular periods a good sign of fertility? Well, it’s a common question, and the answer isn’t always straightforward. At EIRMED, we help folks with all kinds of fertility needs, offering supplements and treatments for both guys and gals. In this piece, we’ll chat about what your menstrual cycle really tells you about getting pregnant, how it all works, and some tips to boost your chances. We’ll keep it simple so anyone can follow along.
 Regular periods show up every 21 to 35 days, last about the same each time, and have a flow that’s not too much or too little. Mild cramps are normal, but nothing that knocks you out. This steady pattern suggests your hormones, like estrogen and progesterone, are doing their job right.
Regular periods show up every 21 to 35 days, last about the same each time, and have a flow that’s not too much or too little. Mild cramps are normal, but nothing that knocks you out. This steady pattern suggests your hormones, like estrogen and progesterone, are doing their job right. Are regular periods a good sign of fertility? If you’re thinking about starting a family or just curious about your body’s signals, this question might have crossed your mind. Regular periods often suggest that your hormones are in balance and your body is preparing for a possible pregnancy each month. But let’s take it step by step. At EIRMED, we focus on helping people like you with
Are regular periods a good sign of fertility? If you’re thinking about starting a family or just curious about your body’s signals, this question might have crossed your mind. Regular periods often suggest that your hormones are in balance and your body is preparing for a possible pregnancy each month. But let’s take it step by step. At EIRMED, we focus on helping people like you with  Hormones are the conductors of your cycle. Follicle-stimulating hormone (FSH) kickstarts egg growth, while luteinizing hormone (LH) triggers release. Estrogen builds the uterine lining, and progesterone maintains it for implantation. Imbalances can cause issues even with regular periods.
Hormones are the conductors of your cycle. Follicle-stimulating hormone (FSH) kickstarts egg growth, while luteinizing hormone (LH) triggers release. Estrogen builds the uterine lining, and progesterone maintains it for implantation. Imbalances can cause issues even with regular periods.
 A Mosaicism Embryo is something you might hear about during IVF, and it can sound confusing at first. Don’t worry, we’re here to explain it clearly. At EIRMED, we want to help you understand your fertility options and feel hopeful. We also offer products like vitamins for women’s egg health or supplements for men’s sperm quality to support you. This guide breaks down everything about mosaic embryos in simple words, so you can talk to your doctor with confidence.
A Mosaicism Embryo is something you might hear about during IVF, and it can sound confusing at first. Don’t worry, we’re here to explain it clearly. At EIRMED, we want to help you understand your fertility options and feel hopeful. We also offer products like vitamins for women’s egg health or supplements for men’s sperm quality to support you. This guide breaks down everything about mosaic embryos in simple words, so you can talk to your doctor with confidence. So, what is a mosaic embryo? It’s an embryo with some normal cells and some cells that have the wrong number of chromosomes. Think of it like a puzzle where most pieces fit, but a few are different. Doctors find this during IVF with a test called PGT-A, where they check a tiny piece of the embryo on day 5 or 6.
So, what is a mosaic embryo? It’s an embryo with some normal cells and some cells that have the wrong number of chromosomes. Think of it like a puzzle where most pieces fit, but a few are different. Doctors find this during IVF with a test called PGT-A, where they check a tiny piece of the embryo on day 5 or 6. Embryo mosaicism means an embryo has two types of cells: some with the right number of chromosomes (46) and some with too many or too few. It’s like having a mix of regular and odd-shaped beads in a necklace. This happens early, when the embryo is just starting to divide after the egg and sperm join.
Embryo mosaicism means an embryo has two types of cells: some with the right number of chromosomes (46) and some with too many or too few. It’s like having a mix of regular and odd-shaped beads in a necklace. This happens early, when the embryo is just starting to divide after the egg and sperm join. Mosaic embryos are embryos with both normal and not-so-normal cells. They’re kind of in the middle—not perfect, but not all wrong either. The term “mosaic” means a mix, like tiles in a colorful pattern. In IVF, doctors spot this when they test embryos to see if they’re good for transfer.
Mosaic embryos are embryos with both normal and not-so-normal cells. They’re kind of in the middle—not perfect, but not all wrong either. The term “mosaic” means a mix, like tiles in a colorful pattern. In IVF, doctors spot this when they test embryos to see if they’re good for transfer.
 How to do in home insemination is a question many people ask when they’re looking for a simple, private way to try for a baby. At EIRMED, we understand that starting or growing your family can feel exciting yet overwhelming, especially if you’re exploring options like this one. Our site helps with fertility medicines and products for both men and women, so you can find what fits your needs. This guide will walk you through everything in clear steps, making sure you have the facts to decide if it’s right for you.
How to do in home insemination is a question many people ask when they’re looking for a simple, private way to try for a baby. At EIRMED, we understand that starting or growing your family can feel exciting yet overwhelming, especially if you’re exploring options like this one. Our site helps with fertility medicines and products for both men and women, so you can find what fits your needs. This guide will walk you through everything in clear steps, making sure you have the facts to decide if it’s right for you. Home insemination means placing sperm into the vagina near the cervix using a simple tool like a syringe, without needing a doctor’s office. It’s a form of artificial insemination you can handle yourself. People often pick this when natural ways aren’t working or when using donor sperm.
Home insemination means placing sperm into the vagina near the cervix using a simple tool like a syringe, without needing a doctor’s office. It’s a form of artificial insemination you can handle yourself. People often pick this when natural ways aren’t working or when using donor sperm. Now, let’s get to the heart of how to do in home insemination. Follow these seven steps carefully for safety and better chances.
Now, let’s get to the heart of how to do in home insemination. Follow these seven steps carefully for safety and better chances.
 How do fertility supplements for women work their magic? It starts with the basics: many contain antioxidants that protect cells from damage, which is key for healthy eggs. Others help regulate hormones, making your cycles more predictable. Imagine your body as a garden, these supplements provide the right soil and water to help things grow.
How do fertility supplements for women work their magic? It starts with the basics: many contain antioxidants that protect cells from damage, which is key for healthy eggs. Others help regulate hormones, making your cycles more predictable. Imagine your body as a garden, these supplements provide the right soil and water to help things grow. Let’s dive into some of the best fertility supplements for women based on current insights from fertility experts and clinics. We’ll cover what each one does, why it might help, and any tips for use. At EIRMED, we stock many of these in forms that are easy to take and backed by quality standards.
Let’s dive into some of the best fertility supplements for women based on current insights from fertility experts and clinics. We’ll cover what each one does, why it might help, and any tips for use. At EIRMED, we stock many of these in forms that are easy to take and backed by quality standards.