Expert Guidance: 10 Science-Backed Keys to Optimizing Intrauterine Insemination (IUI) Success
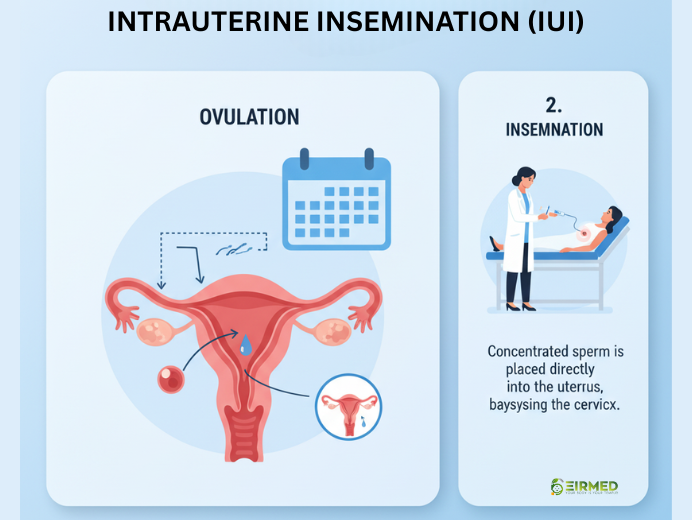
Keys to a successful IUI start with knowing what to do before, during, and after the process. If you are thinking about intrauterine insemination, or IUI, as a way to build your family, you are not alone. Many people turn to this treatment when natural conception is hard. IUI places sperm right into the uterus to help fertilization happen. It is less complex than some other options and can work well for couples dealing with mild fertility issues.
In this guide, we will look at the main factors that can help your IUI go well. We will talk about how to prepare your body, what happens on the day, and tips to care for yourself afterward. As an expert in fertility for both men and women, I want to share this in a simple way, like we are talking over tea. At EIRMED, our site offers products to support your needs, such as supplements for better egg or sperm health.
Introduction: Why Following the Evidence is Key to Fertility Success
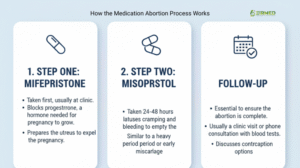
Intrauterine Insemination (IUI) is a popular way to boost the chance of pregnancy. It’s a gentler and often more affordable step before considering complex treatments like In Vitro Fertilization (IVF). In simple terms, IUI involves a doctor placing a concentrated sample of high-quality sperm directly into the patient’s womb (uterus) right around the time the egg is released (ovulation). This procedure helps the sperm skip past the cervix, which is usually a barrier, drastically shortening the distance they need to swim to reach the egg.
Success in IUI isn’t a matter of luck. It depends on carefully planning and perfecting specific factors—including biology, medicine, and procedure steps—that have been proven to work through worldwide clinical studies. By focusing only on the variables with strong scientific proof, patients and their doctors can achieve the best possible results. This report outlines ten research-backed keys that are essential for maximizing the chance of a successful pregnancy with IUI.
Section 1: Clinical Readiness – Getting the Female Body Ready (Keys 1-3)
The first crucial step in making IUI work is checking the female partner’s overall fertility health. These starting biological factors tell doctors how well a patient will react to the treatment and lay the groundwork for the whole cycle.
Key 1: Knowing Your Egg Supply (AMH and AFC)
The total number of eggs a patient has remaining, known as the ovarian reserve, is a very strong sign of how successful fertility treatment will be. Doctors use two main measurements to find this out: Anti-Müllerian Hormone (AMH) and Antral Follicle Count (AFC).
The AMH test is a quick blood test that gives the most dependable estimate of how many eggs a patient still has. Studies show a clear connection: when AMH levels are high, the chances of IUI success are also higher. One important study found that the chance of clinical pregnancy was twice as high (20.0%) when the patient’s AMH level was greater than 2.1 ng/mL, compared to cycles where the level was lower (10.0%). This simply means that women with a good supply of eggs have a much better likelihood of getting pregnant with IUI.
The Antral Follicle Count (AFC) is used alongside AMH. This count is done using an ultrasound to check how many small, resting egg sacs (follicles) are in the ovaries at the start of the menstrual cycle. A higher AFC means there are more potential eggs that can be encouraged to grow during the stimulation phase. Research confirms that patients who achieve a clinical pregnancy tend to have a noticeably higher mean AFC (about 4.0) compared to those who don’t (about 3.2), with the best starting point often being 3.5.
Checking AMH and AFC before treatment is an essential strategic move. If a patient’s AMH is very low (far below 2.1 ng/mL), it suggests a risk of a Poor Ovarian Response (POR). In these cases, even using strong medications (Key 4) often leads to limited success (sometimes as low as 9.2% in certain treatment groups). For patients with very low egg reserves, IUI might be a waste of valuable time, and they should immediately think about moving to IVF. These markers are not just tests; they are vital tools for creating a personalized treatment plan.
Key 2: The Age Factor: Timing Your Treatment Efficiently
A patient’s age is widely known as the most important biological factor affecting IUI results. This is because the quality and quantity of eggs naturally drop over time, making it much harder to achieve a successful pregnancy as a patient gets older.
The data clearly shows that IUI success rates continuously decrease with age. For women under 35 years old, the IUI success rate per cycle is at its highest, around 13%. This rate dips to 10% for women aged 35 to 37 years. The drop becomes steeper after age 38, with success rates falling to 9%, and decreasing further to between 3% and 9% for patients over 40 years.
This age-related decline dictates the entire treatment strategy. Since time is limited, especially for women aged 38 and above, treatment must be very efficient. For example, spending four to six cycles on a treatment that only offers a 3% to 9% chance per cycle is statistically inefficient compared to quickly switching to a treatment with a higher success rate, like IVF. The goal is to choose the most effective treatment plan as quickly as possible to counter the natural decline in egg quality.
Key 3: Preparing the Uterus: Aiming for Optimal Endometrial Thickness (EST)
For a fertilized egg to turn into a baby, the lining of the uterus, called the endometrium, must be perfectly ready to accept and support it. The thickness of this lining (EST) is a crucial physical measurement for success in any assisted reproductive procedure, including IUI. If the endometrium is too thin, it may not have the necessary blood flow and support for the egg to implant successfully.
Research has set clear limits for the uterine lining. Studies show an absolute failure zone: no pregnancies occurred when the peak EST was measured at less than 5.1 mm or greater than 15 mm. This means that if the lining falls outside this critical range, the chance of success is zero, no matter how good the sperm or egg are.
For the best outcomes, most doctors aim for an EST that is in the “sweet spot.” A lining of 7 mm to 12 mm is generally linked to higher pregnancy and implantation rates, with 8 mm often seen as the minimum thickness required to move forward with the procedure.
Monitoring the endometrial thickness is therefore a required check before the IUI is performed. Since success is impossible outside the critical thresholds, checking the lining is mandatory. If the lining is poor (e.g., less than 7 mm), the cycle should be stopped or changed, as a perfect insemination performed into an unsuitable environment will always fail.
Section 2: Treatment Optimization – Protocols and Precision (Keys 4-5)
The next keys focus on getting the medical treatments and steps exactly right during the IUI cycle itself.
Key 4: Boosting Egg Production: Choosing the Best Stimulation Protocol
A key part of IUI success, especially for unexplained infertility, is controlled ovarian stimulation (COS). This uses medication to encourage the growth of several healthy eggs in one cycle. The drug protocol chosen directly affects the number and quality of the eggs produced.
Scientific evidence strongly supports using protocols that aggressively promote follicle growth. Overall studies have shown that using Gonadotropins alone resulted in higher pregnancy rates (33.33%) compared to regimens combining clomiPHENE Citrate (CC) with Gonadotropins (18.36%). This indicates that a stronger medication strategy generally leads to a better chance of clinical pregnancy.2
The best results are seen when aggressive stimulation matches the patient’s capacity. For women who already showed a high ovarian reserve (AMH greater than 2.1 ng/mL, as seen in Key 1), using a comprehensive stimulation protocol—which includes Clomiphene, human gonadotropins, and an hCG trigger (ChmghCG)—resulted in the highest success rate of 32.1%.
This high success rate proves that using strong drugs works best when the patient’s underlying biology is strong. If a patient’s egg capacity is low (low AMH), using aggressive drugs may not help much, which supports the idea of either using a simpler, cheaper stimulation or moving directly to IVF. For a patient with strong markers, using the optimal, aggressive protocol is the best way to leverage her natural potential.
Key 5: Perfect Timing: Triggering Ovulation and Insemination Exactly Right
Once the ovaries have been properly stimulated (Key 4) and the eggs are the right size, the exact timing of the next two steps—the ovulation trigger shot and the sperm injection—is absolutely vital. The egg is only able to be fertilized for a very small window after it is released.
The process begins with an injection of human chorionic gonadotropin (hCG), often called the trigger shot, which causes the final maturation and release of the egg. The IUI procedure must then be strictly scheduled to happen about 36 hours after the hCG trigger shot.9 This timing is essential to ensure that the concentrated sperm sample is already waiting in the fallopian tube precisely when the egg is released, maximizing the chances of fertilization.
Because the window of opportunity is so narrow, the procedure’s timing is non-negotiable. Research suggests that any delay or mistake in scheduling the IUI relative to the hCG injection can significantly lower the success rate. Even with the best eggs and sperm, incorrect timing guarantees failure, which is why sticking to the 36-hour rule is one of the most critical, yet completely controllable, factors for IUI success.
Section 3: The Sperm Factor and Procedural Excellence (Keys 6-7)
IUI is mainly designed to help sperm reach the egg. Therefore, the quality of the sperm sample and the technical skill used in the procedure are extremely important.
Key 6: The Total Motile Sperm Count (TMSC) Rule: Quality Over Quantity
The quality of the prepared sperm sample, measured by the number of actively swimming sperm, is the biggest male predictor of IUI success. This is known as the Total Motile Sperm Count (TMSC), which is the number of active, moving sperm measured after the sample has been washed and concentrated, right before the insemination.
While a few pregnancies have been reported with very low counts, the evidence shows that success rates improve dramatically once the TMSC hits a certain level. Pregnancy rates are significantly better when the post-wash TMSC is at least 5 million. This 5 million mark acts as a crucial minimum for being a good candidate for IUI.
For patients aiming for the highest possible success rate, current research suggests that the chance of pregnancy is best when the TMSC is 9 million or higher. On the flip side, success rates drop sharply when the count is very low; the monthly success rate falls to just 5.3% when the TMSC is below 1 million.
The TMSC is the ultimate check for male fertility issues. If the post-wash count consistently falls below 5 million, IUI is statistically not worth the effort. For couples dealing with severe male infertility, personalized advice should strongly recommend moving to more advanced techniques like IVF with Intracytoplasmic Sperm Injection (ICSI), where the need for high motility is bypassed.
Key 7: Accurate Procedure: Ensuring Gentle and Smooth Insemination
The actual process of injecting the prepared sperm into the uterus demands technical precision to maximize the chance of success.
The main goal of the procedure is to smoothly and completely deposit the concentrated sperm into the uterine cavity, avoiding any damage or the possibility of the sperm flowing back out. Studies have looked into whether the type of catheter used—such as a soft-tip versus a hard-tip—affects the results, but large trials found no significant difference in pregnancy or live birth rates between the two types.
This finding suggests that the specific tool used is less important than the skill and technique of the doctor performing the IUI. The most important technical factor is ensuring the sperm delivery is gentle and accurate. A rough procedure could cause the uterus to contract, which might push the sperm out or prevent its journey toward the fallopian tube. Additionally, standard care often includes resting quietly (lying down) for about 20 minutes after the procedure and receiving luteal support (progesterone) to help keep the uterine environment favorable.
Section 4: Health and Context – Controllable and Non-Controllable Variables (Keys 8-9)
IUI success is closely linked to the patient’s general health and any existing medical conditions. Lifestyle choices can directly affect how well medication works, while specific diagnoses can make the procedure useless.
Key 8: Lifestyle Check: Stopping Smoking and Cutting Back on Alcohol
Lifestyle factors, which are completely controlled by the patient, play a significant role in how effectively the body responds to treatment drugs and prepares the uterus.
Smoking: The scientific evidence against smoking during fertility treatment is very strong. Studies show that patients who smoke need a significantly higher dose of gonadotropin drugs to achieve the same level of ovarian stimulation compared to non-smokers. This increases both the cost and the burden of the treatment. Furthermore, smoking is known to harm the implantation environment by causing a thinner endometrium (EST). A thin lining directly goes against the need for optimal EST (Key 3). By quitting smoking, a patient improves her body’s drug response (Key 4) and enhances the quality of the implantation site (Key 3). Quitting smoking is one of the most effective ways a patient can reduce costs and boost success.
Alcohol: While research found no major link between moderate caffeine intake and fertility success, the findings on alcohol consumption are clearer. A high level of weekly alcohol consumption by women (specifically, greater than 84 grams per week, which is about six standard drinks) is negatively linked to the chance of pregnancy in assisted reproductive technologies. Similarly, high weekly consumption in men (over 84 grams per week) is associated with a decreased live birth rate.
BMI Context: It is important to note that a review of multiple studies on female Body Mass Index (BMI) found that having a high BMI did not statistically change IUI treatment outcomes (clinical pregnancy or live birth rates). Nevertheless, advice on weight loss is often still given to women with a high BMI to lower general pregnancy risks.
Key 9: The Right Treatment for the Right Problem: Knowing IUI’s Limits
IUI is an excellent treatment for specific problems, most often unexplained infertility (the diagnosis in 50.1% of successful cycles studied) and cases where there are issues with sperm delivery. However, IUI is medically ineffective in cases involving severe physical problems within the female reproductive system.
IUI relies on the fundamental step of sperm naturally meeting the egg in the fallopian tube for fertilization. Therefore, the procedure is severely limited, or completely unsuitable, for patients who have:
- Moderate to severe endometriosis.
- Severe fallopian tube disease (such as blocked tubes).
- Severe male factor infertility (where the TMSC is too low, as discussed in Key 6).
- A history of multiple pelvic infections.
For patients diagnosed with conditions known to damage fertility (e.g., tubal disease, diminished ovarian reserve), evaluation and treatment should start right away. Continuing IUI when a structural issue exists—like a severely blocked fallopian tube—is scientifically pointless because the sperm cannot reach the egg. This key emphasizes that the initial diagnosis must be a critical checklist item to confirm IUI is the right choice before starting any cycle.
Section 5: Strategic Planning for Long-Term Success (Key 10)
Key 10: The Smart Pivot: Setting a Limit on IUI Cycles
A defining characteristic of a successful fertility journey is knowing when a treatment strategy has reached its peak and confidently moving on to a more effective option. This choice must be based on age and cumulative results, not just emotion.
Fertility specialists generally agree that patients should attempt between 3 and 6 unsuccessful IUI cycles before seriously thinking about moving on to IVF . For women under 35 with no major issues, three to four cycles offer a total success rate of up to 20% to 30% . However, research clearly shows that after four unsuccessful attempts, the chance of success drops significantly .
The cycle limit must be adjusted according to age (Key 2):
| Maternal Age Group | Recommended Limit of Unsuccessful Cycles | Why the Limit is Set (Strategic Rationale) |
| Under 35 years | 3 to 4 cycles | Total success is decent; there is less urgency to rush. |
| 35 to 37 years | 2 to 3 cycles | Age-related decline begins; efficiency must be prioritized. |
| 38 years and older | 1 to 2 cycles, or skip IUI entirely | Rapid drop in egg quality; low success chance per cycle (3-9%). |
The reason for setting this limit is the principle of diminishing returns. Continuing past the recommended limit wastes precious time, particularly for older patients. Since IVF offers a much higher chance of success per cycle, moving to it is not giving up, but rather a logical, evidence-based step toward the ultimate goal of achieving a live birth. Moving to IVF is also strongly recommended sooner if a patient has limited egg reserve (Key 1) or if multiple high-quality IUI attempts (Keys 4, 5, 6) have failed.
Conclusion and Summary of Scientific Thresholds

The road to a successful IUI cycle is built not just on hope, but on strict adherence to clinical evidence and scientific thresholds. By making the most of biological capacity, ensuring procedural accuracy, and following strict diagnostic rules, couples can significantly increase their chances of success.
The tables below summarize the critical, research-backed numerical targets that define an optimized IUI cycle.
Table 1: Key Female Fertility Markers and IUI Success Thresholds
| Marker (Simple Term) | Clinical Measurement | Optimal Target for Best Success | Critical Threshold (High Risk/Failure) |
| Egg Reserve (AMH) | Anti-Müllerian Hormone (ng/mL) | Greater than 2.1 ng/mL | Below 2.1 ng/mL |
| Follicle Potential (AFC) | Antral Follicle Count | Greater than 3.5 | N/A |
| Uterine Lining (EST) | Endometrial Thickness (mm) | 7 mm to 12 mm | Below 5.1 mm or above 15 mm |
Table 2: Total Motile Sperm Count (TMSC) and IUI Success
| Post-Wash TMSC Range (Millions) | Expected Outcome | Clinical Recommendation |
| Less than 1 million | Very low monthly chance (around 5.3%) | Usually advised to move to IVF/ICSI |
| 5 million or higher | Good candidate profile for IUI (> |
Standard recommendation |
| 9 million or higher | Optimized chance for IUI pregnancy | Best predictive range |
In summary, a successful IUI cycle needs perfect coordination: the patient must have enough eggs (Key 1), be in the appropriate age range (Key 2), have a healthy uterine lining (Key 3), use the strongest possible stimulation protocol (Key 4), perform the insemination at exactly the right time (Key 5), use a strong sperm sample (Key 6), ensure gentle technique (Key 7), follow positive lifestyle habits (Key 8), be an appropriate candidate free of severe structural defects (Key 9), and have the strategic wisdom to switch to IVF when necessary (Key 10). Following these science-backed steps provides the best possible foundation for success.
Recommended YouTube Video on Keys to a Successful IUI
As a fertility expert at EIRMED, I often recommend trusted videos from board-certified doctors to help couples understand IUI better. These align with what top fertility sites like CCRM and Illume Fertility cover—focusing on preparation, timing, and tips for higher success rates. Here’s a standout one:
Video Link: Maximize Your Chances for Getting Pregnant with Intrauterine Insemination – Dr. Lora Shahine
Sumary of Video: In this 10-minute video, reproductive endocrinologist Dr. Lora Shahine shares practical steps to boost IUI success, including who it’s best for, how the procedure works, and key factors like ovulation timing and lifestyle tweaks. It’s straightforward and hopeful, perfect for couples starting their journey—much like the expert advice we provide at EIRMED for male and female fertility support.
Frequently Asked Questions (FAQ) on IUI Success
Q1. What is the best age range for IUI? How does my age affect my chances of getting pregnant with IUI?
Age is the single most important factor determining IUI success, as egg quality and quantity naturally decrease over time.
Generally, success rates are highest for younger patients and drop significantly as a woman ages:
- Under 35 years: The IUI success rate is highest, averaging around 13% per cycle.
- 35 to 37 years: The success rate dips to about 10% per cycle.
- 38 to 40 years: The rate drops further to approximately 9% per cycle.
- Over 40 years: The success rate is lowest, falling into the 3% to 9% range per cycle.
This continuous decline is why doctors often recommend moving to more advanced treatment (IVF) much sooner for patients over 38.
Q2. What is the lowest acceptable sperm count for IUI to still work?
Doctors measure the quality of the sperm sample after it has been washed and prepared, using a number called the Total Motile Sperm Count (TMSC)—the total number of actively swimming sperm.
While some rare pregnancies occur even with very low counts, research shows that success rates are significantly better when the TMSC is at least 5 million. If the TMSC is 5 million or higher, the pregnancy rate is typically 8.2% or more per cycle.
For the best possible chance of success with IUI, the optimal TMSC is 9 million or higher. If the TMSC drops below 1 million, the monthly chance of success falls sharply to only 5.3%, suggesting that IVF/ICSI may be a more efficient option.
Q3. What AMH level do I need for IUI to be successful?
The Anti-Müllerian Hormone (AMH) blood test is the best way to estimate your remaining egg supply (ovarian reserve).
Research has identified a crucial cut-off point of 2.1 ng/mL. Having an AMH level greater than 2.1 ng/mL is associated with a much higher probability of success. Specifically, cycles where the patient’s AMH was above this number had a pregnancy rate of 20.0%, which is double the rate (10.0%) seen in cycles where the AMH level was below 2.1 ng/mL.
For patients with an AMH level above 2.1 ng/mL, using a strong stimulation protocol (like Gonadotropins) can further boost the success rate to 32.1%.
Q4. Is there a limit on how many IUI cycles I should try before moving to IVF?
Yes, most fertility experts recommend setting a limit because the chance of success drops significantly after a certain number of attempts.
The limit is strongly dependent on the patient’s age:
| Maternal Age Group | Recommended Limit of Unsuccessful Cycles | Rationale |
| Under 35 years | 3 to 4 cycles | These cycles offer a decent total success rate (up to 20–30%). |
| 35 to 37 years | 2 to 3 cycles | Moving to IVF sooner is recommended due to the age-related decline in egg quality. |
| 38 years and older | 1 to 2 cycles, or skip IUI | It is often recommended to move quickly to IVF due to the rapid decline in egg quality and very low success rates (3-9%). |
If you have completed the recommended number of cycles for your age without success, transitioning to IVF is seen as the next logical and more efficient step.
Q5. What is the perfect uterine lining thickness (EST) for a successful IUI?
The uterine lining, or endometrium (EST), must be ready to receive the fertilized egg.
- Optimal “Sweet Spot”: A lining thickness between 8 mm and 12 mm is generally associated with the highest pregnancy and implantation rates. A thickness of 7 mm to 8 mm is usually viewed as the minimum threshold for proceeding with the procedure.
- Absolute Failure Zone: Studies show that no pregnancies occurred when the peak EST was measured at less than 5.1 mm or greater than 15 mm. If your lining falls outside this crucial range, the cycle will likely fail.
Q6. Should I quit smoking and drinking alcohol before starting IUI?
Yes, absolutely. Lifestyle choices you can control play a major role in success:
- Smoking: Patients who smoke are required to use a significantly higher dosage of fertility drugs (gonadotropins) to achieve the same stimulation results as non-smokers. Smoking also leads to a thinner endometrium , which is counterproductive to achieving the optimal uterine lining (Key 5).
- Alcohol: High weekly alcohol consumption by women (specifically, more than 84 grams per week, about six standard drinks) has been found to be negatively associated with pregnancy rates in fertility treatments. Men’s consumption above the same threshold (84g per week) is associated with a decreased live birth rate.
Quitting smoking and limiting alcohol intake are proven ways to improve your body’s response to medication and prepare the uterus for pregnancy.
Q7. What diagnosis makes IUI not recommended?
IUI is most helpful for couples with unexplained infertility or issues with sperm delivery. However, IUI is ineffective when there are severe structural problems that prevent the sperm and egg from meeting.
IUI has the lowest success rates and is often not recommended if you have:
- Moderate to severe endometriosis.
- Severe fallopian tube disease (such as tubes that are blocked).
- A history of multiple pelvic infections.
- Very severe male factor infertility (where the prepared sperm count is too low, specifically below 5 million TMSC).
For patients with these conditions, doctors generally advise moving directly to IVF, as IUI is scientifically unlikely to succeed
Overall Purpose
This article aims to share simple, helpful facts on keys to a successful IUI. It helps people understand the process, prepare their bodies, and care for themselves after. By covering health checks, lifestyle tips, and emotional support, it meets what users search for. The goal is to make fertility journeys easier and more hopeful. At EIRMED, we want you to feel informed and ready to buy products that fit your needs, like supplements for better results. Stay positive—many find success with these steps.
Disclaimer
This content is for general information only and not medical advice. Always talk to a doctor for personal guidance on fertility treatments. EIRMED does not diagnose or treat conditions. Results vary by person. We are not liable for any actions based on this article. Seek professional help for your health needs.
Thank You
Thank you for reading this guide on keys to a successful IUI. We hope it gives you hope and clear steps for your fertility path. At EIRMED, we are here to support you with quality products. Remember, every journey is unique, and you are taking brave steps. Wishing you all the best.

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.








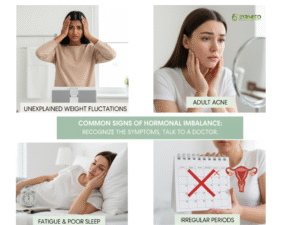 You may not know your hormones are off until you try to get pregnant. Look for these common signs. Irregular periods are a big clue – maybe they come too often or skip months. You could feel very tired all the time, even after sleep. Mood swings, like feeling sad or angry for no reason, happen too.
You may not know your hormones are off until you try to get pregnant. Look for these common signs. Irregular periods are a big clue – maybe they come too often or skip months. You could feel very tired all the time, even after sleep. Mood swings, like feeling sad or angry for no reason, happen too.
 Yes, it is important to address hormonal imbalances even if pregnancy is not a current goal. Hormones regulate far more than fertility—they influence mood, metabolism, heart health, bone strength, and cognitive function. Leaving a hormonal imbalance untreated can increase the risk of long-term health issues such as thyroid disease, osteoporosis, or metabolic disorders.
Yes, it is important to address hormonal imbalances even if pregnancy is not a current goal. Hormones regulate far more than fertility—they influence mood, metabolism, heart health, bone strength, and cognitive function. Leaving a hormonal imbalance untreated can increase the risk of long-term health issues such as thyroid disease, osteoporosis, or metabolic disorders.
 Myth 1: Frequent Self-Stimulation Causes Low Sperm Count or Infertility (Azoospermia)
Myth 1: Frequent Self-Stimulation Causes Low Sperm Count or Infertility (Azoospermia)


 For many women, the surgery is a straightforward, life-changing decision that offers peace of mind. However, when your period doesn’t show up as expected afterward, it’s completely natural to panic and think, “Wait, is this possible?”
For many women, the surgery is a straightforward, life-changing decision that offers peace of mind. However, when your period doesn’t show up as expected afterward, it’s completely natural to panic and think, “Wait, is this possible?”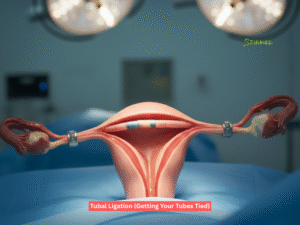 The Simple Job of the Fallopian Tubes
The Simple Job of the Fallopian Tubes If you miss your period after getting your tubes tied, it’s natural to panic, but medically, doctors look at several common, non-pregnancy reasons first. (Source: Mayo Clinic, Johns Hopkins Medicine)
If you miss your period after getting your tubes tied, it’s natural to panic, but medically, doctors look at several common, non-pregnancy reasons first. (Source: Mayo Clinic, Johns Hopkins Medicine)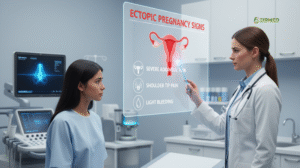
 Because tubal ligation is meant to be permanent, reversing the surgery is often difficult and not very successful.
Because tubal ligation is meant to be permanent, reversing the surgery is often difficult and not very successful.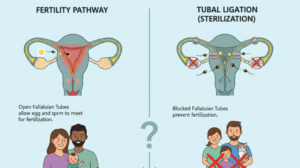

 Let us be clear right away: You do not need to have an orgasm to get
Let us be clear right away: You do not need to have an orgasm to get  These uterine contractions are stimulated by a sudden, powerful release of the hormone oxytocin. Oxytocin is known as the “love hormone” because it promotes bonding, but it is also a powerful factor in the reproductive system (it’s the same hormone used to induce labor).
These uterine contractions are stimulated by a sudden, powerful release of the hormone oxytocin. Oxytocin is known as the “love hormone” because it promotes bonding, but it is also a powerful factor in the reproductive system (it’s the same hormone used to induce labor).

 The simple answer is that your body is a sperm-making factory that works 24/7. However, for a single sperm cell to go from its very beginning stage to a fully mature, ejaculation-ready “swimmer,” the complete process known as spermatogenesis, takes an average of 64 to 74 days (roughly 2.5 to 3 months).
The simple answer is that your body is a sperm-making factory that works 24/7. However, for a single sperm cell to go from its very beginning stage to a fully mature, ejaculation-ready “swimmer,” the complete process known as spermatogenesis, takes an average of 64 to 74 days (roughly 2.5 to 3 months). Your lifestyle choices are the most powerful factors determining the quality of your newly regenerated sperm.
Your lifestyle choices are the most powerful factors determining the quality of your newly regenerated sperm. This comparison highlights why men have such a fantastic opportunity to influence their fertility in a relatively short period. If you and your partner are on a treatment path, adopting these changes for the next 90 days can be your greatest contribution to the effort. Even centers like the Center for Reproductive Medicine emphasize the importance of men being fully engaged in the preparation phase.
This comparison highlights why men have such a fantastic opportunity to influence their fertility in a relatively short period. If you and your partner are on a treatment path, adopting these changes for the next 90 days can be your greatest contribution to the effort. Even centers like the Center for Reproductive Medicine emphasize the importance of men being fully engaged in the preparation phase.