The Ultimate 10-Point Guide: Foods to Avoid While Taking Letrozole for Fertility
Hello again from EIRMED! We know that using a medicine like Letrozole for fertility is a big part of your life right now. You’re doing everything right by focusing on your diet, because what you eat can truly support your success.
This detailed guide goes beyond the basics to explain exactly why certain foods and habits should be avoided. Our goal is to give you the most optimized, easy-to-read, and complete information so you can give your body the very best chance to ovulate and conceive.
Understanding Letrozole | How Food Plays a Role
Let’s start with a quick reminder. Letrozole is an oral pill that is a non-steroidal Aromatase Inhibitor.
- Its Mission: To lower your body’s estrogen levels for a short time.
- The Result: Your brain notices the low estrogen and releases a high amount of Follicle-Stimulating Hormone (FSH), which helps your ovaries grow a nice, mature egg for ovulation.
When we talk about Foods to Avoid While Taking Letrozole for Fertility, we are looking at anything that:
- Interferes with how your body breaks down Letrozole (making the dose too high or too low).
- Works against the medicine by trying to raise estrogen levels.
- Makes the side effects of the medicine (like hot flashes or nausea) much worse.
The Top 10 Things to Avoid While Taking Letrozole
 For the best results with your Letrozole for fertility cycle, pay close attention to the following 10 points.
For the best results with your Letrozole for fertility cycle, pay close attention to the following 10 points.
1. Grapefruit and Grapefruit Juice
Grapefruit is the most serious concern when taking many medications, including Letrozole.
- The Deep Detail: Grapefruit contains compounds that block a crucial liver enzyme called CYP3A4. This enzyme is like the “cleanup crew” for many drugs, including Letrozole. When the cleanup crew is blocked, the Letrozole stays in your body for too long.
- The Risk: This increases the concentration of the drug in your blood, which can lead to stronger, more severe side effects, or worse, make the medicine act differently than your doctor intended.
- Action Plan: Strictly avoid grapefruit, grapefruit juice, and all related fruits like pomelos, tangelos, and Seville oranges for the entire month you are taking Letrozole.
2. Excessive Soy Products (The Estrogen Mimic)
Soy is famous for containing phytoestrogens, plant compounds that act like weak estrogen in the body.
- The Deep Detail: Since Letrozole’s job is to lower estrogen, eating large amounts of soy might slightly reduce the medicine’s effectiveness by putting a little bit of “estrogen” back into your system.
- The Risk: For fertility, high intake may confuse your body’s signalling, making the FSH release less effective.
- Action Plan: Limit or avoid high-concentration soy products like soy protein powders, soy milk (in large quantities), and soy supplements. Small, whole-food portions like a few cubes of tofu or a bowl of edamame are usually fine, but cut back on the heavily processed stuff.
3. High Saturated and Trans Fats (Cholesterol and PCOS Link)
This is especially important if you are taking Letrozole for fertility due to PCOS.
- The Deep Detail: Letrozole can sometimes cause an increase in your cholesterol levels. Furthermore, studies on Letrozole-induced PCOS models (in labs) show that a high-fat diet can make the metabolic issues related to PCOS, like insulin resistance, much worse.
- The Risk: Increased bad cholesterol and worsening insulin resistance can make it harder for your hormones to balance out, potentially reducing the success rate of the drug.
- Action Plan: Avoid foods high in saturated fats like fatty red meats, full-fat dairy (switch to low-fat or plant-based), butter, and all processed foods with trans fats (e.g., many baked goods and fried foods).
4. Excessive Caffeine (The Sleep and Anxiety Multiplier)
While caffeine does not directly stop Letrozole from working, it definitely works against your well-being.
- The Deep Detail: Letrozole can cause headaches, hot flashes, and difficulty sleeping. Caffeine makes all of these side effects worse. Poor sleep affects every hormone in your body and makes you feel exhausted and irritable during a stressful treatment cycle.
- The Risk: High intake (over 200mg/day) may also be associated with negative pregnancy outcomes later on.
- Action Plan: Reduce to one small cup of coffee (or tea) in the morning only. Switch to decaf or herbal teas later in the day to protect your sleep.
5. Alcohol (Liver Load and Embryo Safety)
Drinking alcohol is counterproductive to the fertility journey.
- The Deep Detail: Your liver is busy processing Letrozole. Adding alcohol puts extra strain on your liver. More importantly, alcohol should be avoided entirely once you ovulate (the luteal phase) because it can harm a developing embryo.
- The Risk: Worsens side effects (nausea, dizziness) and risks the potential pregnancy.
- Action Plan: Avoid alcohol entirely while you are undergoing any fertility treatment.
6. Refined Carbohydrates and Simple Sugars (Worsening Insulin Resistance)
If you have PCOS, this category is almost as important as grapefruit.
- The Deep Detail: Simple carbs (white rice, white bread, sugary drinks, candy) spike your blood sugar very quickly. If you have insulin resistance (common with PCOS), this causes a surge of insulin, which, in turn, boosts male hormones (androgens) that stop ovulation.
- The Risk: High sugar actively fights the hormone environment Letrozole is trying to create.
- Action Plan: Replace these with complex, high-fiber carbs like whole grains (quinoa, oats, brown rice) and vegetables.
7. Unapproved Herbal Supplements (Hormone Hijackers)
This is a hidden danger often found in health food stores.
- The Deep Detail: Many herbs (like Black Cohosh, Dong Quai, Red Clover, and Maca) are sold to help “balance hormones” or treat menopausal symptoms, but they often contain compounds that act like estrogen.
- The Risk: These supplements can directly block the estrogen-lowering effect of Letrozole, making your cycle completely ineffective.
- Action Plan: Never take any herbal or natural supplement without specific approval from your fertility doctor. Prenatal vitamins and basic Vitamin D are usually safe, but check first!
8. High-Sodium and Processed Foods (Bloating and Bone Health)
These foods relate to common side effects of treatment.
- The Deep Detail: Letrozole can cause some people to feel bloated or retain water. High sodium intake makes this fluid retention much worse. Long-term use of Letrozole can also affect bone density, and high sodium is known to affect calcium balance.
- The Risk: Increased discomfort and potential long-term risks if you are on multiple cycles.
- Action Plan: Minimize fast food, salty packaged snacks, and pre-made frozen meals.
9. Spicy Foods (Worsening Hot Flashes)
A simple change for a common side effect.
- The Deep Detail: Hot flashes are one of the most common side effects of Letrozole because the drug lowers estrogen, which regulates body temperature. Spicy food raises your core body temperature.
- The Risk: Eating very spicy meals can trigger or worsen uncomfortable hot flashes, especially at night.
- Action Plan: Limit very spicy dishes during the 5 days you take the pill and the week after.
10. Highly Acidic Foods (If You Have Nausea)
A simple comfort rule.
- The Deep Detail: Some people feel mild nausea or an upset stomach when taking Letrozole. Highly acidic foods like concentrated tomato sauce, citrus juices (aside from grapefruit), and vinegar can make an already sensitive stomach feel worse.
- The Risk: Increased nausea and discomfort.
- Action Plan: If you feel nauseous, try taking your pill with a bland snack (like toast) and avoid highly acidic foods during that time.
Diet Support for Your Letrozole Cycle
 Now that we know what to avoid, here is a quick table on what to choose to help your treatment succeed!
Now that we know what to avoid, here is a quick table on what to choose to help your treatment succeed!
What People Are Asking About Letrozole and Diet
We’ve reviewed common questions patients ask their doctors about Foods to Avoid While Taking Letrozole for Fertility.
Letrozole Success and Supplements: What Is Safe?
Does Letrozole Cause Weight Gain, and How Does Diet Prevent It?
It’s true that some women report weight changes while on Letrozole, though it’s not guaranteed. The reason is usually hormone changes and fluid retention.
- How Diet Helps: By strictly avoiding refined sugars and saturated fats, you keep your calorie intake and blood sugar stable. The best way to prevent weight gain on Letrozole is to follow a healthy, balanced diet based on whole foods, similar to the Mediterranean diet, and keep up with light, regular exercise.
Overall Purpose
Your journey with Letrozole for fertility is about taking the right pill at the right time and supporting it with smart food choices. Remember the top priority is Grapefruit, followed by limiting large amounts of high-estrogen foods (like soy protein) and high-sugar items. When you choose fresh, whole, and unprocessed foods, you are helping Letrozole work better, making your body healthier for ovulation, and increasing your chance of a successful pregnancy.
Frequently Asked Questions (FAQ)
Q1: Can I still eat beans and lentils while taking Letrozole?
A: Yes, absolutely. Beans and lentils are fantastic sources of protein and fiber, which are great for stabilizing blood sugar (especially good for PCOS). While some lists mention them due to very low-level phytoestrogens, the health benefits far outweigh any minor risk. Focus on including them!
Q2: I sometimes get headaches on Letrozole. What should I drink instead of coffee?
A: Headaches are common because of the hormone change. Stay super hydrated with water first. You can also try naturally caffeine-free drinks like peppermint tea, ginger tea (which may help with nausea), or sparkling water with a slice of lemon.
Q3: How long does Letrozole stay in my system after I stop taking the 5-day dose?
A: Letrozole is cleared from your system quite quickly. Most of the drug is gone within about 45 hours (less than two days) after your last pill. However, the effects on your hormones last longer, which is what causes ovulation. It’s best to maintain your smart dietary choices until you know the result of the cycle.
Disclaimer
This article is provided by EIRMED for educational purposes only and should not be used as a substitute for consulting with your personal fertility specialist or healthcare provider. Always discuss your diet, any supplements, and all medications with your doctor before starting or changing your treatment plan.
Thank you for choosing EIRMED for your fertility information. We are cheering you on

Eirmed is an informational platform dedicated to providing reliable, science-based insights on male and female fertility, reproductive health, and natural conception.


 If you’re reading this, it means your heart has changed its mind. You may have chosen to get your tubes tied, the procedure called tubal ligation in the past, thinking your family was complete. But life often brings new dreams, new partners, or a desire to hold another child. Now, you have a huge question burning in your mind: “Can you untie your tubes?”
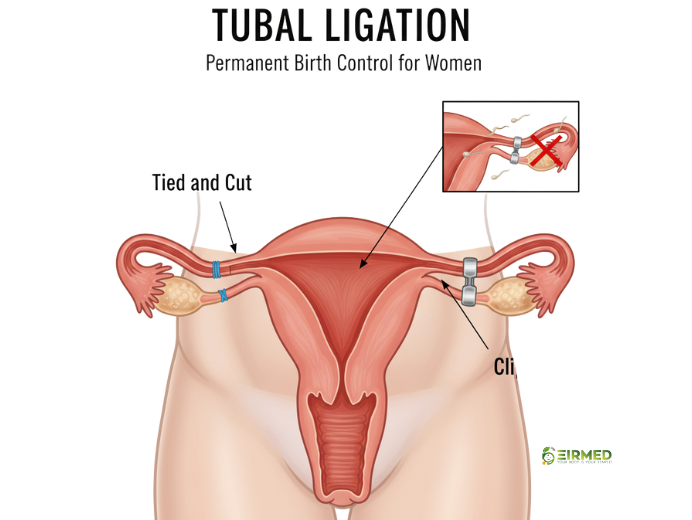
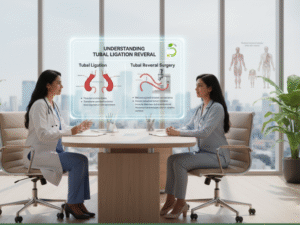
If you’re reading this, it means your heart has changed its mind. You may have chosen to get your tubes tied, the procedure called tubal ligation in the past, thinking your family was complete. But life often brings new dreams, new partners, or a desire to hold another child. Now, you have a huge question burning in your mind: “Can you untie your tubes?”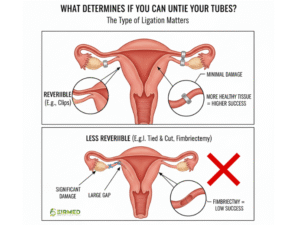 The very first step in determining if a tubal reversal surgery is possible is knowing how your tubes were tied. The success of the reversal hinges entirely on how much healthy fallopian tube is left to repair.
The very first step in determining if a tubal reversal surgery is possible is knowing how your tubes were tied. The success of the reversal hinges entirely on how much healthy fallopian tube is left to repair.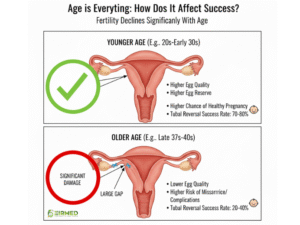 When you’re considering a
When you’re considering a 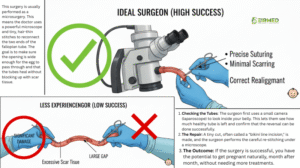 A
A 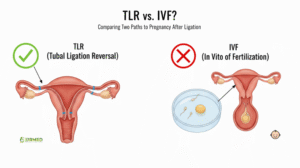 Money is a practical reality in every family-building decision. When deciding if you can you untie your tubes, you must compare the cost of reversal surgery to the cost of In Vitro Fertilization (IVF).
Money is a practical reality in every family-building decision. When deciding if you can you untie your tubes, you must compare the cost of reversal surgery to the cost of In Vitro Fertilization (IVF).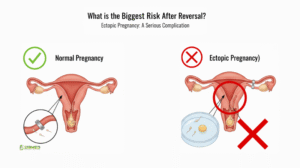 You must understand the most important risk when you try to get pregnant after a
You must understand the most important risk when you try to get pregnant after a 
 Throughout history, the symbolism of colors has woven through various cultures, embodying the essence of fertility and life’s renewal. Consider ancient Egypt, where the color green adorned the god Osiris, symbolizing the rejuvenation brought by the fertile silt of the Nile. What color represents fertility? This question often arises when people consider symbols of new life, growth, and hope. In many cultures around the world, colors hold deep meanings associated with fertility.
Throughout history, the symbolism of colors has woven through various cultures, embodying the essence of fertility and life’s renewal. Consider ancient Egypt, where the color green adorned the god Osiris, symbolizing the rejuvenation brought by the fertile silt of the Nile. What color represents fertility? This question often arises when people consider symbols of new life, growth, and hope. In many cultures around the world, colors hold deep meanings associated with fertility. Long ago, people used colors to tell stories about life and birth. In ancient times, the color associated with fertility often came from nature. For example, early humans associated green with fields where crops grew well, linking it to an abundance of food and children. In Egypt, the god Osiris was depicted with green skin, symbolizing rebirth and the fertility of the land along the Nile River. In other places, such as India, red has been a symbol of fertility for thousands of years. Brides wear red to wish for a happy marriage and many kids. This demonstrates that colors are not just aesthetically pleasing; they carry power in shaping beliefs. Today, we still see these ideas in holidays, art, and even medical spaces. At fertility clinics, soft colors like blue might calm patients during treatments.
Long ago, people used colors to tell stories about life and birth. In ancient times, the color associated with fertility often came from nature. For example, early humans associated green with fields where crops grew well, linking it to an abundance of food and children. In Egypt, the god Osiris was depicted with green skin, symbolizing rebirth and the fertility of the land along the Nile River. In other places, such as India, red has been a symbol of fertility for thousands of years. Brides wear red to wish for a happy marriage and many kids. This demonstrates that colors are not just aesthetically pleasing; they carry power in shaping beliefs. Today, we still see these ideas in holidays, art, and even medical spaces. At fertility clinics, soft colors like blue might calm patients during treatments. In today’s world, colors are used in fertility clinics to create welcoming spaces. Soft greens and blues help patients relax during exams or treatments. Some doctors suggest color therapy, where you surround yourself with vibrant hues to boost your mood and mindset.
In today’s world, colors are used in fertility clinics to create welcoming spaces. Soft greens and blues help patients relax during exams or treatments. Some doctors suggest color therapy, where you surround yourself with vibrant hues to boost your mood and mindset.
 If you’ve been trying to start a family and things feel off, fertility hormone imbalance in both male and female bodies might be the quiet reason behind it. Hormones are like the body’s messengers, guiding everything from egg release in women to sperm production in men. When these signals get mixed up, it can make conception tougher than it should be. But here’s the good news: understanding this early opens doors to simple fixes and hopeful journeys. At EIRMED, we see so many couples turn things around with the right knowledge and support. Let’s walk through what this means for you, step by step, so you feel less alone and more in charge.
If you’ve been trying to start a family and things feel off, fertility hormone imbalance in both male and female bodies might be the quiet reason behind it. Hormones are like the body’s messengers, guiding everything from egg release in women to sperm production in men. When these signals get mixed up, it can make conception tougher than it should be. But here’s the good news: understanding this early opens doors to simple fixes and hopeful journeys. At EIRMED, we see so many couples turn things around with the right knowledge and support. Let’s walk through what this means for you, step by step, so you feel less alone and more in charge. Hormones keep our reproductive systems running smoothly, but when levels shift too high or too low it creates a ripple effect. For women, this often ties to conditions like polycystic ovary syndrome (PCOS), where male-like hormones called androgens build up and block regular ovulation. In men, low testosterone can slow sperm creation, leading to fewer or weaker swimmers. This imbalance isn’t rare; it affects up to 10% of women of childbearing age and a similar share of men facing fertility challenges.
Hormones keep our reproductive systems running smoothly, but when levels shift too high or too low it creates a ripple effect. For women, this often ties to conditions like polycystic ovary syndrome (PCOS), where male-like hormones called androgens build up and block regular ovulation. In men, low testosterone can slow sperm creation, leading to fewer or weaker swimmers. This imbalance isn’t rare; it affects up to 10% of women of childbearing age and a similar share of men facing fertility challenges. For women, the triggers often start with the ovaries and brain signals. PCOS tops the list, caused by genes, insulin resistance (when your body doesn’t use sugar well), or inflammation from diet. Thyroid problems, either underactive (hypothyroidism) or overactive mess with estrogen and progesterone, the key players in monthly cycles. Age plays a role too; as you near 35, natural dips in follicle-stimulating hormone (FSH) can signal perimenopause sneaking in early.
For women, the triggers often start with the ovaries and brain signals. PCOS tops the list, caused by genes, insulin resistance (when your body doesn’t use sugar well), or inflammation from diet. Thyroid problems, either underactive (hypothyroidism) or overactive mess with estrogen and progesterone, the key players in monthly cycles. Age plays a role too; as you near 35, natural dips in follicle-stimulating hormone (FSH) can signal perimenopause sneaking in early. Symptoms whisper before they shout, but listening early saves heartache. Fertility hormone imbalance shows up differently in men and women, yet both share that nagging sense something’s not right.
Symptoms whisper before they shout, but listening early saves heartache. Fertility hormone imbalance shows up differently in men and women, yet both share that nagging sense something’s not right.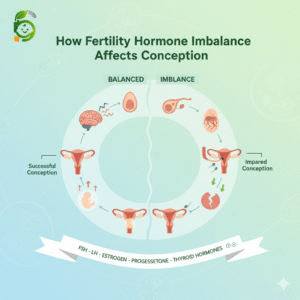 When
When 
 What is sperm morphology? It refers to the shape and size of sperm cells. This aspect of male fertility reveals a great deal about how effectively sperm can reach and unite with an egg. Many people are unfamiliar with it, but understanding it can be beneficial if you are planning a family. At EIRMED, our site focuses on fertility for men and women. We offer medicines and treatments to support your needs, like supplements for better sperm health. In this guide, we will explain everything in simple words. We want you to feel informed and hopeful.
What is sperm morphology? It refers to the shape and size of sperm cells. This aspect of male fertility reveals a great deal about how effectively sperm can reach and unite with an egg. Many people are unfamiliar with it, but understanding it can be beneficial if you are planning a family. At EIRMED, our site focuses on fertility for men and women. We offer medicines and treatments to support your needs, like supplements for better sperm health. In this guide, we will explain everything in simple words. We want you to feel informed and hopeful. Sperm morphology looks at the head, middle part, and tail of each sperm. The head holds the DNA, which is the information needed for a baby. It should be oval and smooth. The middle part gives energy for swimming. The tail helps it move forward like a whip. When we ask, ‘What is sperm morphology?’ we mean checking if these parts are formed correctly.
Sperm morphology looks at the head, middle part, and tail of each sperm. The head holds the DNA, which is the information needed for a baby. It should be oval and smooth. The middle part gives energy for swimming. The tail helps it move forward like a whip. When we ask, ‘What is sperm morphology?’ we mean checking if these parts are formed correctly. How to get pregnant with poor sperm morphology? This question worries many couples trying to have a baby.
How to get pregnant with poor sperm morphology? This question worries many couples trying to have a baby.  What could be behind those unusual sperm shapes? Several things can lead to abnormal sperm morphology, also known as teratozoospermia. Genetics plays a role; some men inherit traits that affect the form of their sperm. Environmental factors, such as exposure to toxins like pesticides or heavy metals, can also alter sperm structure.
What could be behind those unusual sperm shapes? Several things can lead to abnormal sperm morphology, also known as teratozoospermia. Genetics plays a role; some men inherit traits that affect the form of their sperm. Environmental factors, such as exposure to toxins like pesticides or heavy metals, can also alter sperm structure. Testing is easy and key to understanding what
Testing is easy and key to understanding what  Good news: You can often make sperm morphology better. Start with healthy eating. Foods rich in fruits, vegetables, nuts, and fish are beneficial. They give antioxidants to protect sperm.
Good news: You can often make sperm morphology better. Start with healthy eating. Foods rich in fruits, vegetables, nuts, and fish are beneficial. They give antioxidants to protect sperm.
 Reasons for blocked tubes can be a confusing and emotional topic if you’re facing fertility challenges. These tubes play a key role in getting pregnant, acting as the path where eggs and sperm meet. If they’re blocked, it might stop that from happening naturally. At EIRMED, we focus on helping you understand these issues so you can make smart choices about your health. Let’s explore the common causes, signs, and ways to handle them, all in a way that’s easy to follow and supportive.
Reasons for blocked tubes can be a confusing and emotional topic if you’re facing fertility challenges. These tubes play a key role in getting pregnant, acting as the path where eggs and sperm meet. If they’re blocked, it might stop that from happening naturally. At EIRMED, we focus on helping you understand these issues so you can make smart choices about your health. Let’s explore the common causes, signs, and ways to handle them, all in a way that’s easy to follow and supportive.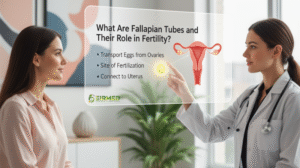 Fallopian tubes are slim passages linking your ovaries to your uterus. Each month, an egg moves through them, hoping to meet sperm for fertilization. When things go right, the fertilized egg travels to the uterus to grow into a baby. But if there’s a blockage, it can lead to infertility. Understanding fallopian tube problems is crucial because they affect about 25-30% of infertility cases in women, based on insights from fertility experts like those at the
Fallopian tubes are slim passages linking your ovaries to your uterus. Each month, an egg moves through them, hoping to meet sperm for fertilization. When things go right, the fertilized egg travels to the uterus to grow into a baby. But if there’s a blockage, it can lead to infertility. Understanding fallopian tube problems is crucial because they affect about 25-30% of infertility cases in women, based on insights from fertility experts like those at the 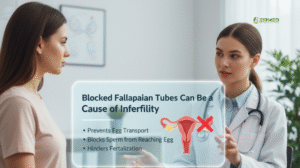
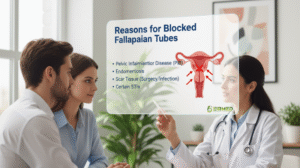 Diving deeper, reasons for blocked fallopian tubes include past infections beyond PID, like those from miscarriages or abortions. Scar tissue from pelvic surgeries or conditions such as irritable bowel syndrome can compress the tubes. Congenital issues, where tubes are abnormal from birth, are rare but possible. Unexplained blockages happen, too, frustrating many women. Competitor insights from Illume Fertility and PFCLA emphasize that STIs and endometriosis are frequent culprits, urging regular check-ups to catch problems early.
Diving deeper, reasons for blocked fallopian tubes include past infections beyond PID, like those from miscarriages or abortions. Scar tissue from pelvic surgeries or conditions such as irritable bowel syndrome can compress the tubes. Congenital issues, where tubes are abnormal from birth, are rare but possible. Unexplained blockages happen, too, frustrating many women. Competitor insights from Illume Fertility and PFCLA emphasize that STIs and endometriosis are frequent culprits, urging regular check-ups to catch problems early.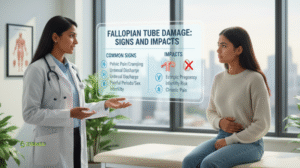
 Closed fallopian tubes mean complete blockage, often from severe scarring or hydrosalpinx. This fully stops natural conception on that side. If both are closed, IVF becomes key. Insights from CNY
Closed fallopian tubes mean complete blockage, often from severe scarring or hydrosalpinx. This fully stops natural conception on that side. If both are closed, IVF becomes key. Insights from CNY  To avoid blockages, treat STIs promptly, use protection, and undergo regular gynecological exams. Avoid smoking, which harms reproductive health. Maintain a healthy weight to reduce your risk of endometriosis. Insights from Medical News Today suggest that lifestyle changes can lower the chances of infection, protecting tubes in the long term.
To avoid blockages, treat STIs promptly, use protection, and undergo regular gynecological exams. Avoid smoking, which harms reproductive health. Maintain a healthy weight to reduce your risk of endometriosis. Insights from Medical News Today suggest that lifestyle changes can lower the chances of infection, protecting tubes in the long term.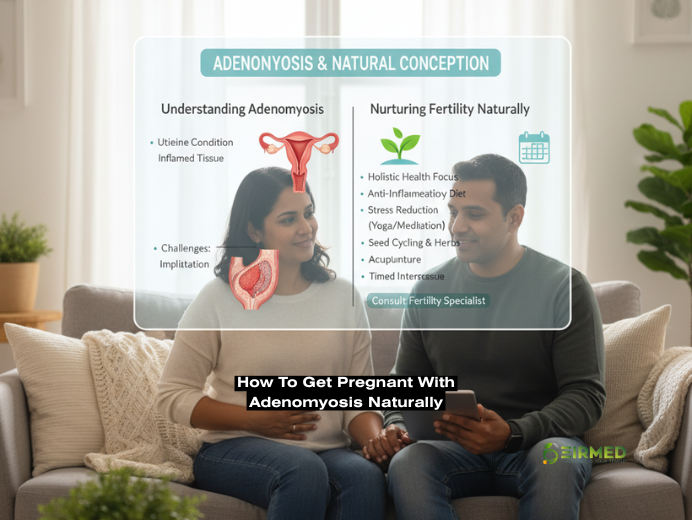
 How to get pregnant with adenomyosis naturally is a question many women ask when facing this common yet challenging condition. It involves the inner lining of the uterus growing into its muscular wall, leading to discomfort that can disrupt daily life and dreams of starting a family. But you are not alone in this; countless women have found ways to support their bodies and achieve pregnancy through gentle, everyday adjustments.
How to get pregnant with adenomyosis naturally is a question many women ask when facing this common yet challenging condition. It involves the inner lining of the uterus growing into its muscular wall, leading to discomfort that can disrupt daily life and dreams of starting a family. But you are not alone in this; countless women have found ways to support their bodies and achieve pregnancy through gentle, everyday adjustments. Adenomyosis occurs when endometrial tissue, which should only line the uterus, invades the muscle layer, causing the uterus to enlarge and become tender. This can lead to heavier periods and ongoing discomfort, affecting about one in ten women, often in their 30s or 40s. Based on information from reliable sources, the condition stems from factors like prior uterine surgeries or hormonal shifts, creating an environment where inflammation thrives. Unlike endometriosis, where tissue grows outside the uterus, adenomyosis stays within, but both can overlap, complicating matters. Recognizing early signs helps in planning ahead, especially if family-building is on your mind.
Adenomyosis occurs when endometrial tissue, which should only line the uterus, invades the muscle layer, causing the uterus to enlarge and become tender. This can lead to heavier periods and ongoing discomfort, affecting about one in ten women, often in their 30s or 40s. Based on information from reliable sources, the condition stems from factors like prior uterine surgeries or hormonal shifts, creating an environment where inflammation thrives. Unlike endometriosis, where tissue grows outside the uterus, adenomyosis stays within, but both can overlap, complicating matters. Recognizing early signs helps in planning ahead, especially if family-building is on your mind. Understanding the stages of adenomyosis can help you gauge its progression and seek timely support. In the early stage
Understanding the stages of adenomyosis can help you gauge its progression and seek timely support. In the early stage Yes, you can get pregnant with adenomyosis, though it may require extra patience and care. Studies indicate that while the condition can reduce implantation success by up to 30%, many women conceive naturally or with assistance. The thickened uterine wall may hinder embryo attachment, but factors such as age and symptom severity also play a role. Women who’ve shared their journeys often highlight how addressing inflammation improved their odds. If you’ve been trying for months without success, consulting a specialist can clarify your unique situation, combining natural approaches with monitoring for optimal outcomes.
Yes, you can get pregnant with adenomyosis, though it may require extra patience and care. Studies indicate that while the condition can reduce implantation success by up to 30%, many women conceive naturally or with assistance. The thickened uterine wall may hinder embryo attachment, but factors such as age and symptom severity also play a role. Women who’ve shared their journeys often highlight how addressing inflammation improved their odds. If you’ve been trying for months without success, consulting a specialist can clarify your unique situation, combining natural approaches with monitoring for optimal outcomes. How I cured my adenomyosis without surgery often involves non-invasive options like UAE or hormonal therapies, but many opt for natural routes. Women report relief through a consistent diet and acupuncture, avoiding operations while improving fertility.
How I cured my adenomyosis without surgery often involves non-invasive options like UAE or hormonal therapies, but many opt for natural routes. Women report relief through a consistent diet and acupuncture, avoiding operations while improving fertility.

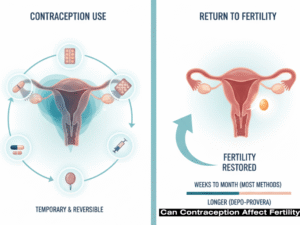 Can contraception affect fertility? This is a concern many women face when considering or stopping birth control, wondering if methods like pills or IUDs might hinder future pregnancies. The truth is, most forms of contraception are reversible and do not cause lasting infertility, allowing fertility to return soon after discontinuation. In this comprehensive guide, we’ll delve into the science behind contraception, its temporary effects on your cycle, common misconceptions, and practical steps to support your reproductive health. Drawing from trusted medical sources, we’ll address how different methods work and what you can expect when planning a family.
Can contraception affect fertility? This is a concern many women face when considering or stopping birth control, wondering if methods like pills or IUDs might hinder future pregnancies. The truth is, most forms of contraception are reversible and do not cause lasting infertility, allowing fertility to return soon after discontinuation. In this comprehensive guide, we’ll delve into the science behind contraception, its temporary effects on your cycle, common misconceptions, and practical steps to support your reproductive health. Drawing from trusted medical sources, we’ll address how different methods work and what you can expect when planning a family. Different birth control options have unique profiles, but none lead to long-term infertility. Let’s examine how each might influence your cycle after stopping.
Different birth control options have unique profiles, but none lead to long-term infertility. Let’s examine how each might influence your cycle after stopping. Depo-Provera injections provide three-month protection but can delay fertility recovery up to 18 months. Still, they do not cause permanent infertility. Implants like Nexplanon allow quicker returns, often within a month. Recovery rates reach 82.9% within a year for similar injectables.
Depo-Provera injections provide three-month protection but can delay fertility recovery up to 18 months. Still, they do not cause permanent infertility. Implants like Nexplanon allow quicker returns, often within a month. Recovery rates reach 82.9% within a year for similar injectables. Yes, short-term disruptions like irregular periods or delayed ovulation are common as hormones stabilize. This phase varies by method, with injectables taking longest. Monitoring cycles helps identify when fertility returns.
Yes, short-term disruptions like irregular periods or delayed ovulation are common as hormones stabilize. This phase varies by method, with injectables taking longest. Monitoring cycles helps identify when fertility returns. Many myths persist, but evidence shows no long-term harm. Birth control does not lead to weight gain causing infertility or damage fertility permanently. It won’t make future pregnancies harder. Misconceptions often stem from outdated fears.
Many myths persist, but evidence shows no long-term harm. Birth control does not lead to weight gain causing infertility or damage fertility permanently. It won’t make future pregnancies harder. Misconceptions often stem from outdated fears.
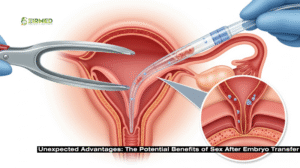 Here’s where it gets interesting: sex after embryo transfer isn’t always a no-go. Some evidence suggests it could even help. Seminal fluid packs proteins, hormones, and immune factors that signal the uterus to be more receptive. A randomized trial on FET cycles found that intercourse the night before transfer upped clinical pregnancy rates by about 24%, likely due to these immune-modulating effects. It’s like nature’s way of prepping the ground, similar to natural pregnancies where semen exposure aids implantation.
Here’s where it gets interesting: sex after embryo transfer isn’t always a no-go. Some evidence suggests it could even help. Seminal fluid packs proteins, hormones, and immune factors that signal the uterus to be more receptive. A randomized trial on FET cycles found that intercourse the night before transfer upped clinical pregnancy rates by about 24%, likely due to these immune-modulating effects. It’s like nature’s way of prepping the ground, similar to natural pregnancies where semen exposure aids implantation. Balance is key, so let’s talk risks. Orgasms trigger uterine contractions, which might dislodge an unattached embryo. One study linked intercourse during the 5-10 day implantation window to higher miscarriage odds, especially if repeated in that week. Infections pose another threat, as the transfer can breach cervical mucus, and introducing bacteria increases the chances, though rare at about 1-2%.
Balance is key, so let’s talk risks. Orgasms trigger uterine contractions, which might dislodge an unattached embryo. One study linked intercourse during the 5-10 day implantation window to higher miscarriage odds, especially if repeated in that week. Infections pose another threat, as the transfer can breach cervical mucus, and introducing bacteria increases the chances, though rare at about 1-2%.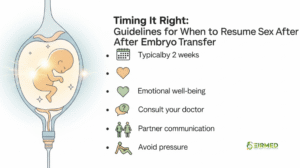 Most advice? Hold off 48 hours to 7-14 days
Most advice? Hold off 48 hours to 7-14 days  IVF strains bonds, and pausing sex after embryo transfer can amplify feelings of distance. But it’s an opportunity to nurture non-physical closeness. Research links
IVF strains bonds, and pausing sex after embryo transfer can amplify feelings of distance. But it’s an opportunity to nurture non-physical closeness. Research links 
 Signs a man is fertile can offer reassuring clues about reproductive health, especially when you’re
Signs a man is fertile can offer reassuring clues about reproductive health, especially when you’re  Male fertility involves producing enough healthy sperm to travel effectively to fertilize an egg.
Male fertility involves producing enough healthy sperm to travel effectively to fertilize an egg.  One strong sign a man is fertile is having testicles that feel normal, about the size of a walnut, firm but not hard, without pain or swelling.
One strong sign a man is fertile is having testicles that feel normal, about the size of a walnut, firm but not hard, without pain or swelling.  Balanced facial and body hair growth is another clue to hormone levels that
Balanced facial and body hair growth is another clue to hormone levels that  Look for semen that’s white or grey, about 1.5 to 5 millilitres per ejaculation, roughly a teaspoon and slightly thick at first.
Look for semen that’s white or grey, about 1.5 to 5 millilitres per ejaculation, roughly a teaspoon and slightly thick at first.  Feeling energetic throughout the day? That’s a good sign a man is fertile, linked to balanced hormones and good circulation for sperm health. Low energy might stem from poor sleep or obesity, which can cut sperm motility.
Feeling energetic throughout the day? That’s a good sign a man is fertile, linked to balanced hormones and good circulation for sperm health. Low energy might stem from poor sleep or obesity, which can cut sperm motility. A stable mood without constant stress is tied to lower cortisol, which otherwise harms sperm production. Frequent mood swings or depression could indicate hormonal shifts affecting fertility.
A stable mood without constant stress is tied to lower cortisol, which otherwise harms sperm production. Frequent mood swings or depression could indicate hormonal shifts affecting fertility. A healthy sex drive with no issues like erectile dysfunction is a direct sign that a man is fertile, showing solid blood flow and hormones. Problems here might relate to low desire or ejaculation troubles.
A healthy sex drive with no issues like erectile dysfunction is a direct sign that a man is fertile, showing solid blood flow and hormones. Problems here might relate to low desire or ejaculation troubles.